REVIEW ARTICLE
Maintenance Fluids in Pediatric Practice: What has Changed?

Piyush Gupta, MD, FAMS
Professor,Department of Pediatrics, University College of Medical Sciences, Delhi
Nidhi Bedi, MD
Assistant Professor, Department of Pediatrics, Jamia Hamdard Institute of Medical Sciences and Research, Delhi
Correspondence to: Dr Piyush Gupta, Professor, Department of Pediatrics, University College of Medical Sciences, Delhi 110095. Email: prof.piyush.gupta@gmail.com
For last 200 years human science has beentrying to understand the concept behind basic fluid requirement for an individual. It all started way back in 1832 when Lancetreported its first case on use of fluid therapy. And today, with release of the American Academy of Pediatrics Guidelines on Maintenance fluids in December 2018, the initial concepts have taken a complete U-turn.
Historical Review
Fluid therapy made its first appearance almost 20 decades back when Lattareported the first case on use of fluid therapy in Lancet in 1832[1]. In 1878 Bernardintroduced the concept of internal milieu.Further,Gamble et al (1940) were the firstto introduce the concept of ECF (Extracellular fluid) as enclosed sea which was later found to be more like gel rather than sea[2]. The next major understanding was made by Darrow et al[3] who provided a major concept to maintenance fluid therapy. He tied the “maintenance” allowance of water in a 24-hour period to metabolic rate rather than to the body weight. This concept laid the basis for the Holiday-Segar method[4], used till date to calculate maintenance fluid requirement.
Physiology of Body Water
Total body water content in humans changes significantly with age. Starting at almost 80% of body weight at birth, it decreases to 60% at the end of first year of life and to 50-60% by adult age. The proportion of extracellular and intracellular fluid also varies with age. At birth 45% of total body weight is extracellular water whereas 35% of total body weight is intracellular water. As the child grows to become an adult, about 20% of total body weight is extracellular water and 40% is intracellular water[5,6].
Maintenance therapy refers to the provision of fluid and electrolytes to replace anticipated losses from breathing, sweating, and urine output. It is needed by the average individual with normal ICF/ECF volumes over a 24-hour period[7]. Water is continuously lost from the body through the skin, lungs and kidneys and intermittently from the gastrointestinal tract. The insensible water loss is the volume of fluid which leaves the body as a result of the difference in vapor pressure between the skin and lung surfaces and the surrounding atmosphere[8]. This difference is largely determined by the temperature of the skin and lung surfaces which is further dependent on the metabolic rate. On an average, a rise in body temperature of 1-degree C will increase the insensible water loss by approximately 10 percent[8].
Higher metabolic rate, more body surface area to weight ratio, increasedpercentage of total body water to weightand high respiratory rates predisposes children to higher fluid requirement than adults.
Evolution of Present day Maintenance Therapy
Holliday-Segar method has been the most common technique to calculate maintenance fluids for children.This method was primarily meant to estimate kilocalories lost. Since it was found that 1 kilocalorie requires 1 mL in replacement, the same calculation was efficiently used to calculate fluid requirements (Table 1). As far as composition of intravenous fluids was concerned, maintenance electrolyte requirements in children after various calculations were found to be 3 mEq of sodium, 2 mEq of chloride, and 2 mEq of potassium for every 100 mL of maintenance IV fluid. Considering these, the best suitable intravenous fluid in children became 0.18% NaCl in 5% Dextrose plus 20 mEq/L of potassium chloride[9]. So, for years together children have been administered hypotonic fluids based on above calculations. Till a few years back, we were also using Isolyte-P/Kidral P for routine maintenance therapy in children
Over last two decades it was realized that the dose and type of fluid during the 4 phases of fluid therapy (Table 2) need to be adjusted based on the physiologic needs of each individual and a fixed protocol cannot be applied to all[10]. Dextrose, once considered to increase the tonicity of the fluids, is no more considered to be a significant contributor to the plasma osmotic pressure or tonicity in the absence of uncontrolled diabetes because it rapidly metabolizes after entering the blood stream[10].
Hyponatremia with Hypotonic Fluid
Multiple cases across the world have been reported in previous years on rising incidence of symptomatichyponatremia in children receivinghypotonic maintenance fluids, starting right from 1992[11]. Since then more than20randomized controlled trials and 7 systematic reviews including Cochrane review have been published in various journals on risk of hyponatremia with hypotonic solution. The Institute for Safe Medical Practices of United States and Canada in 2009 released reports on deaths from severe hyponatremia in patients who were hospitalized and received hypotonic intravenous fluids[12,13]. The United Kingdom in 2007 also released a national safety alert reporting 4 deaths and 1 near miss from hospital-acquired hyponatremia[14].
Isotonic vs Hypotonic fluids : Before we proceed to understand more about the risk of hyponatremia with hypotonic fluids it is essential to understand the basic difference in isotonic and hypotonic fluids. Isotonic fluid has a sodium concentration similar tothat of plasma. Plasma is approximately 93% aqueous and 7% anhydrous with a sodium concentration in the aqueous phase of plasma of 154 mEq/L and osmolarity of 308 mOsm/L. The sodium concentration of isotonic fluids ranges from 131 to 154 mEq/L depending upon the solution being used. Table 3 provides composition of all the commonly used fluid solutions. Hypotonic fluid has a sodium concentration lower than that of the aqueous phase of plasma[10]. Thus while Normal saline is an Isotonic fluid, half Normal saline or anything less than that is hypotonic!
Various reasons have been cited for the hyponatremic events. The most likely cause is increased release of AVP (arginine vasopressin). A lot of conditions associated in sick children like pain, stress, nausea, hypovolemia can stimulate release of AVP besides medical disorders like pneumonia, meningitis and postoperative state which are already known to increase release of AVP. Increased release of AVP causes impaired free water excretion, as in SIADH, leading to increase in incidence of hyponatremia specially while using hypotonic fluids. Secondly it was noted that when using calorimetric methods, energy expenditure in sick patients averages 50 to 60 kcal/kg per day which is close to their basal metabolic rate and lesser than the routine daily requirement[10]. As a result, some of the researchers also considered hypotonic fluid overload to be an additional factor.Certain patients are already prone to develop hyponatremia such as those with heart disease, liver disease, renal dysfunction, adrenal insufficiency, neurosurgical patients and patients on medications like desmopressin, known to increase AVP release[15,16].
Many clinicians feared the risk of hypernatremia by using isotonic fluids. The same was nulled in multiple studies collated under a Cochrane review in 2014[17]. Following this, in 2015 the National Clinical Guideline Centre in the United Kingdom published its evidence-based guidelines for IVF therapy in children younger than 16 years old and recommended isotonic intravenous fluids[18].
Finally, in April 2016, the American Academy of Pediatrics convened a multidisciplinary committee for a detailed literature review and released its evidence-based guidelines in December 2018. The American Academy of Pediatrics recommends that patients 28 days to 18 years of age requiring maintenance intravenous fluids should receive isotonic solutions with appropriate potassium chloride and dextrose because they significantly decrease the risk of developing hyponatremia. This guideline applies to children in surgical (postoperative) and medical acute-care settings, including critical care and the general inpatient ward. Patients with neurosurgical disorders, congenital or acquired cardiac disease, hepatic disease, cancer, renal dysfunction, diabetes insipidus, voluminous watery diarrhea, or severe burns; neonates who are younger than 28 days old or in the NICU; and adolescents older than 18 years old are excluded[10].
Practical tips based on the current recommendations are summarized in Box 1.
Funding: None.
Competing interests: None stated.
References
- Lata T. Letter from Dr. Latta to the Central Board of Health, London. Relative to the treatment of cholera by the copious injection of aqueous and saline fluids into the vein. Lancet 1832;II:274– 277.
- Gamble JL. Chemical Anatomy, Physiology and Pathology of Extracellular Fluid, Cambridge, MA, Harvard University Press, 1947.
- Darrow DC, Pratt EL. Fluid therapy; Relation to tissue composition and the expenditure of water and electrolyte. JAMA 1950;143:365-373.
- Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics 1957;19:823-832.
- Fanaroff AA, Martin RJ, eds. Neonatal Perinatal Medicine. 7th ed. St. Louis, MO: Mosby, Inc.; 2002.
- Friis-Hansen B. Body water compartments in children: Changes during growth and related changes in body composition. Pediatrics 1961;28:169-81.
- Aaron FL. Pediatric hydration therapy: Historical review and a new approach. Kidney International, Vol. 67 (2005), pp. 380–388
- Levine SZ, Wilson JR, Kelly M. Insensible perspiration in infancy and childhood. Am J Dis Child 1929;37:791–806
- Weil WB. A unified guide to parenteral fluid therapy. I. Maintenance requirements and repair of dehydration. Pediatrics1969;75(1):1-12
- Feld LG, Neuspiel DR, Foster BA, et al. Clinical Practice Guideline: Maintenance Intravenous Fluids in Children. Pediatrics. 2018;142(6):e20183083
- Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304(6836):1218–1222
- ISMP. Medication safety alert. Plain D5W or hypotonic saline solutions post-op could result in acute hyponatremia and death in healthy children. Available at: ismp.org. Accessed on 30 December 2018
- ISMP Canada. Hospital-acquired acute hyponatremia: two reports of pediatric deaths.ISMP Canada Saf Bul. 2009;9(7). Available at: http://www.ismp-canada. org/download/safetyBulletins/ ISMPCSB2009-7-HospitalAcquiredA cuteHyponatremia.pdf. Accessed on 23 December 2018
- National Patient Safety Agency. Reducing the risk of hyponatraemia when administering intravenous infusions to children. 2007. Available at: www.npsa.nhs.uk/health/alerts. Accessed on 27 December 2018
- Wang J, Xu E, Xiao Y. Isotonic versus hypotonic maintenance IV fluids in hospitalized children: a meta-analysis. Pediatrics. 2014;133:105-13.
- Shamim A, Afzal K, Ali SM. Safety and efficacy of isotonic (0.9%) vs. hypotonic (0.18%) saline as maintenance intravenous fluids in children: a randomized controlled trial. Indian Pediatr. 2014;51:969---74.
- McNab S, Ware RS, Neville KA, et al. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. 2014;(12):CD009457
- National Clinical Guideline Centre (UK). IV Fluids in Children: Intravenous Fluid Therapy in Children and Young People in Hospital. London, United Kingdom: National Clinical Guideline Centre; 2015. Available at: www.ncbi.nlm.nih. gov/pubmed/26741016. Accessed on 24 December 2018
Table 1: Holliday Segar Formula for calculating the amount of maintenance fluid
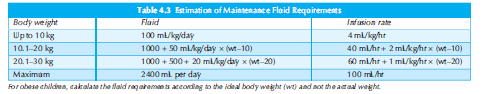
Table 2: Four phases of Fluid Resuscitation
| Resuscitative phase | Fluid boluses to restore adequate tissue perfusion and prevent end-organ injury. |
| Titration phase | IVFs transitioned from boluses to maintenance |
| Maintenance phase | Fluids given to ensure balance between needs and losses |
| Convalescent phase | Intrinsic fluid regulationstartsand exogenous fluids stopped |
Table 3: Composition of commonly used intravenous fluids
| IV fluid | Na+(meq/L) | K+(meq/L) | Cl-(meq/L) | Ca2>+(meq/L) | others |
| Ringer Lactate | 130 | 4 | 109 | 3 | Lactate 28meq/L |
| Normal saline | 154 | - | 154 | - | |
| DNS | 154 | - | 154 | - | Dextrose 50 g/L |
| 0.45 DNS | 77 | - | 77 | - | Dextrose 50 g/L |
| Isolyte P | 25 | 20 | 22 | - | Dextrose 50 g/L, citrate-3meq/L |
Box 1: 2018 Guidelines for Maintenance Fluids
- Maintenance intravenous fluids are needed (if sufficient enteral fluids cannot be provided due to illness/other reasons) to preserve the extracellular volume, prevent depletion of intravascular volume, and minimize the risk of hypo/hypernatremia,
- The osmolarity of plasma is 308 mOsm/L. Osmolarity calculations for IV fluids usually exclude the dextrose in the solution because dextrose is rapidly metabolized in solution.
- Hypotonic fluids for maintenance therapy result in a high incidence of hyponatremia. Hypotonic fluids include N/5 (0.2%) NaCl with 5% dextrose (Osmolarity 78 mOsm/L), and N/2 (0.45%) NaCl with 5% dextrose (Osmolarity 154 mOsm/L).
- Patients between 28 days to 18 years of life should receive isotonic fluid for maintenance fluid therapy with appropriate potassium chloride and dextrose, to reduce the risk of developing hyponatremia. NaCl 0.9 % with 5% dextrose (308 mOsm/L) is an isotonic IV fluid. Ringer lactate with 5% dextrose (273 mOsm/L) is near isotonic.
- These guidelines apply to children in surgical (postoperative) and medical acute care settings, including critical care and the general inpatient ward. Patients with neurosurgical disorders, congenital or acquired cardiac disease, hepatic disease, cancer, renal dysfunction, diabetes insipidus, voluminous watery diarrhea, or severe burns; neonates who are younger than 28 days old or in the NICU; and adolescents older than 18 years old are excluded.
Reference : Clinical Practice Guideline: Maintenance Intravenous Fluids in Children. American Academy of Pediatrics. Pediatrics 2018;142:e20183083. To read full text, click: http://pediatrics.aappublications.org/content/pediatrics/early/2018/11/21/peds.2018-3083.full.pdf

