Snippets
Clinic Practice Guidelines
Pediatric GERD

Diagnosis
- Avoid barium contrast studies, esophago-gastro-duodenoscopy, scintigraphy, and manometry to diagnose GERD in both infants and children
- The diagnosis is mainly by a careful history, physical examination, ruling out other conditions in presence of ‘red flag’ signs; pH-metry and pH impedance studies may be required in few cases to correlate symptoms with episodes of acid reflux events.
- A 4-to-8 week trial of PPIs may be considered as a diagnostic test for typical GERD symptoms in children, but not in infants or in children with extra-gastrointestinal symptoms
Treatment
Infants
- Modify feeding volumes and frequency to avoid overfeeding and use thickened feeds for treating visible regurgitation/vomiting.
- Continue breastfeeding; consider elimination of animal milk protein in mothers in case of non-improvement
- A 2- to 4-week trial of a formula with extensively hydrolyzed protein (or amino-based formula) in formula-fed infants suspected of having GERD after optimal nonpharmacological treatment described above has failed.
- Avoid positional therapy (ie, head elevation, lateral and prone positioning) in sleeping infants.
- Consider 4-8 week trial of acid suppression with H2 antagonists or PPI, then wean if symptoms improved
Children
- Avoid H2RA or PPIs in children with extra-esophageal symptoms (eg, respiratory) except in presence of typical GERD symptoms
- Consider head elevation or left lateral position to treat GERD symptoms.
- Consider 4-8 week trial of acid suppression with H2 antagonists or PPI, then wean if symptoms improved
(Source: 2018 Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). JAMA Pediatr. 2019;173(5):485-486. doi:10.1001/jamapediatrics.2019.0170 )
Guidelines for Maintenance IV Fluids
- Maintenance intravenous fluids are needed (if sufficient enteral fluids cannot be provided due to illness/other reasons) to preserve the extracellular volume, prevent depletion of intravascular volume, and minimize the risk of hypo/hypernatremia,
- The osmolarity of plasma is 308 mOsm/L. Osmolarity calculations for IV fluids usually exclude the dextrose in the solution because dextrose is rapidly metabolized in solution.
- Hypotonic fluids for maintenance therapy result in a high incidence of hyponatremia. Hypotonic fluids include N/5 (0.2%) NaCI with 5% dextrose (Osmolarity 78 mOsm/L), and N/2 (0.45%) NaCI with 5% dextrose (Osmolarity 154 mOsm/L).
- Patients between 28 days to 18 years of life should receive isotonic fluid for maintenance fluid therapy with appropriate potassium chloride and dextrose, to reduce the risk of developing hyponatremia. NaCI 0.9 % with 5% dextrose (308 mOsm/L) is an isotonic IV fluid. Ringer lactate with 5% dextrose (273 mOsm/L) is near isotonic.
- 5.These guidelines applies to children in surgical (postoperative) and medical acute care settings, including critical care and the general inpatient ward. Patients with neurosurgical disorders, congenital or acquired cardiac disease, hepatic disease, cancer, renal dysfunction, diabetes insipidus, voluminous watery diarrhea, or severe burns; neonates who are younger than 28 days old or in the NICU; and adolescents older than 18 years old are excluded.
(Reference: Clinical Practice Guideline: Maintenance Intravenous Fluids in Children. American Academy of Pediatrics. Pediatrics 2018;142:e20183083. To read full text, click: http://pediatrics.aappublications.org/content/pediatrics/early/2018/11/21/peds.2018-3083..full.pdf )
Broad-Spectrum or Narrow Spectrum Antibiotics for Pediatric Acute Bacterial Respiratory Tract Infections
Antibiotics are the most frequently prescribed medications in children, most commonly for otitis media, sinusitis, or pharyngitis. Broad-spectrum antibiotics such as amoxicillin/clavulanate, cephalosporins, and macrolides are increasingly used based on theoretical benefits against emerging resistant pathogens.
Findings
An investigation in USA examined 1 retrospective (n = 30 159) and 1 prospective (n = 2472) cohort, having patients with otitis media, sinusitis, or pharyngitis (aged 6 months to 12 years).
In the retrospective cohort, 14% were prescribed broad-spectrum antibiotics. Analysis found no difference in the primary outcome of treatment failure at 14 days for broad- vs narrow-spectrum antibiotics (3.4% vs 3.1%; risk difference, 0.3%; 95% CI, −0.4% to 0.9%).
The prospective cohort found that patient-centered outcomes were not improved for those receiving broad-spectrum antibiotics (no difference in missed school or daycare; slightly worse quality of life) and that adverse events were higher, whether reported by clinicians (3.7% broad- vs 2.7% narrow-spectrum) or patients (35.6% broad- vs 25.1% narrow-spectrum).
Implications
- Narrow-spectrum antibiotics (eg, penicillin, amoxicillin) should be the mainstays for antibiotic treatment of acute otitis media, acute sinusitis, and group A streptococcal pharyngitis.
- Broad-spectrum antibiotics do not confer additional treatment benefit and may be associated with more adverse events.
Kawasaki Disease: 10 Key Points
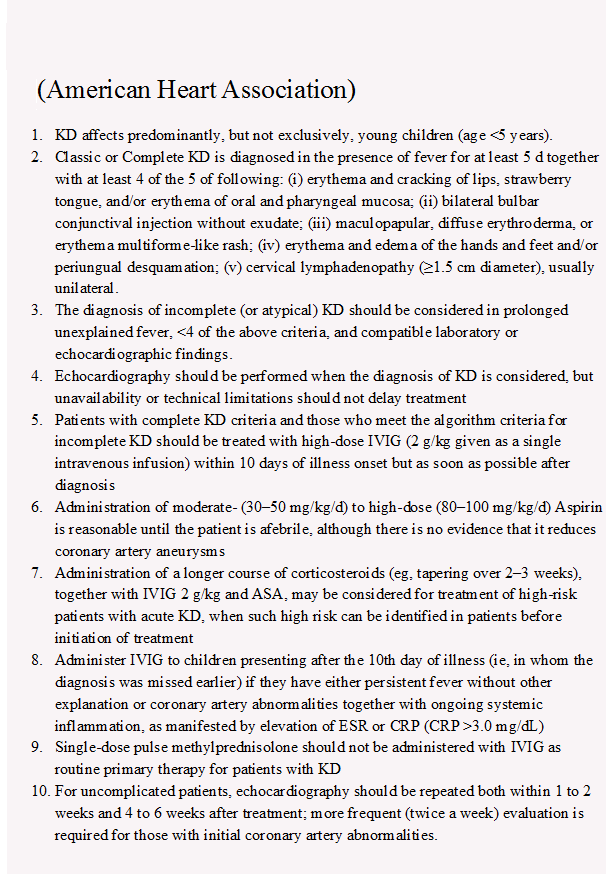
To read full Guildlines : https://www.ahajournals.org/doi/full/10.1161/cir.0000000000000484
(Compiled by: Dr Piyush Gupta, MD, FAMS, Professor of Pediatrics and In-charge, Medical Education Unit, University College of Medical Sciences, Delhi.)

