Update
GLUTEN FREE DIET:
BEYOND AVOIDING WHEAT/BARLEY/RYE AS STAPLE DIET

Strict, lifelong Gluten Free Diet (GFD) is the only treatment available for management of Celiac Disease (CD) currently. Since the damage to the intestinal villi is mediated immunologically, ingestion of even minute amount of gluten precipitates the villi-devastating cascade. Thus, unlike food intolerance (even non-celiac gluten sensitivity), just avoiding wheat, barley and rye in staple diet is not enough in management of Celiac Disease. It is essential to avoid even the minute amounts of ubiquitous gluten. To achieve this, one needs to adopt not only gluten-free staple cereals, but also gluten-free ingredients, gluten free-storage of food items and gluten-free cooking.
This article aims to provide deeper insight and practical tips about gluten-free diet, which is often out of the scope of standard pediatric textbooks, and is essential to maintain gluten free status of your patients of Celiac Disease. Since the incidence of Celiac Disease is increasing (increasing incidence and increased detection) exponentially globally, it is imperative for pediatricians to be aware of the nuances.
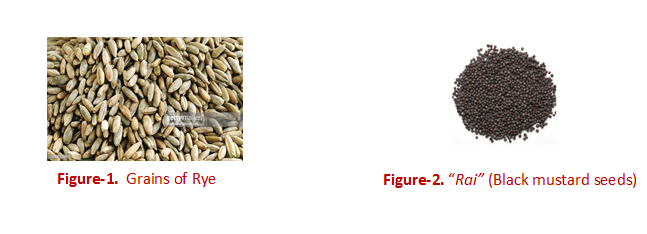
The principle sources of gluten are wheat, rye and barley. It must be clarified that rye is a cereal that looks like wheat (figure-1) and is principally used as a forage food (animal fodder) or for brewing. It is also used to make flour and breads: it is popular in Eastern Europe and is hardly used in India. This clarification is essential for patients since Indians often confuse it with black mustard seeds, since it is called "Rai" (same pronunciation as rye) (figure-2) in Hindi and Gujarati. Black mustard seed ("Rai") is popular in India and is gluten free.
Another common confusion among parents is regarding use of oats as they get divergent opinions on the internet. The confusion is understandable, as the gluten-free status of oats has historically flip-flopped even in academic circles (1) and continues to be debated (2). As such, oats are generally considered gluten-free, but contain avenins that share antigenic epitopes with gluten. This was the reason why oats were initially clubbed with wheat, rye and barley on the allergen list. However, the ability of avenins to trigger the villi-damage is controversial, as many CD patients can tolerate oats without any problem. However, it has increasingly been recognized that it is the contamination of oats with wheat that is the problem. Oat is a winter (rabi) crop just like wheat and is often grown in the same field as wheat and same harvesting and storage equipment is used for it. Further, it is processed on the same equipment line where wheat is also processed. Hence oats are almost always contaminated with minute amounts of wheat. Hernando et al (3) tested 134 samples of various grains and commercial products of oats available in North America, Canada and Europe for gluten. If was found that only 25 of these were devoid of gluten. In 109 samples, the gluten was found at an average of 200 ppm that is 10 times the level that is considered as safe. It has been suggested that even the clinical studies that tried to study tolerance of oats in CD patients might have used the oats that were contaminated (at harvesting/ transportation/ processing stage), thus confounding the results (4). The 2009 European Commission Regulations and 2013 US laws specifically mention that products containing oats can be sold as gluten-free food only if any contamination with gluten is below 20ppm (1). However, the legal status in Australia and New Zealand is different. The authorities there maintain that the tests for gluten do not test for avenin. Hence even the foods with undetectable level of gluten can only be marketed as "wheat-free" and not gluten-free. The position statement of Coeliac Australia on this issue also mentions that some patients with Celiac Disease can adversely react with even uncontaminated oats. They recommend duodenal biopsy before and 3 months after regular consumption of oats to be sure that oats are safe for the Celiac patients who wish to consume oats as a part of Gluten Free diet (5). In view of above and the sad fact that the regulations and degree of law enforcement are poorer in India, I personally don’t advise oats at all as a part of Gluten Free diet. Simply put, patients need to avoid wheat, barley, oats (and rye).
Gluten free diet ideally should be "gluten free": that is, should not have any detectable gluten. The sensitivity of currently available tests for gluten in food is 5ppm and any level below this is reported as "undetectable". This (5ppm) is the cut-off that authorities in Australia/ New Zealand require to be for the food to be labelled as gluten-free. However, the guidelines by the Codex Alimentarius Commission, established by Food and Agricultural Organization (FAO) and World Health Organization (WHO) recommend a cut off of 20ppm. This is followed by most countries globally. The same is notified recently by Government of India in Food Safety and Standards (Food Product Safety and Food Additives) Second Amendment Regulations, 2016. To understand this figure of 20ppm realistic terms, let us take an example of bread. A slice of regular bread roughly weighs 25 grams and it has about 5grams (5000mg) of gluten. Hence, 1/250th (20/5000) of a slice of bread in 1kg of food is damaging for a patient of CD (figure-3)! Thus, even when wheat/ barley/ oats/ rye is not used directly as an ingredient in a food item, it is crucial to know and avoid any ingredient with "hidden gluten", avoid cross-contamination of gluten while cooking/ storing of food and know and avoid other possible sources of gluten other than food per se. Only then the patients of CD can maintain their gluten-free status.
Figure-3. Can you see a grain of regular bread on this plate? If gluten-free bread is served on this plate to a celiac patient, this much gluten is enough to trigger villi-damaging cascade!
Table-1 lists the possible sources of hidden gluten in food ingredients and non-food products. Even some medicines have gluten as a part of excipients. To protect celiac disease patients, many countries have banned gluten across all medicines, while others have made it mandatory to disclose information on gluten on all medicines. Sadly, India has no such policy whatsoever! Unlike FSSAI which has made some steps towards safety of food for celiac disease patients, the Drug Controller is far behind in this direction. In the absence of any information on presence of gluten in medicines, I have not mentioned anything on the subject in table-1. But treating clinicians need to be aware of this source of hidden gluten also (how??)
Table-1 Some examples (not an exhaustive list) of sources of hidden gluten in food ingredients and other products and how to avoid these (adapted from Ref no. 6 and ingredient lists of commercially available packaged food items)
|
Source |
Avoidance/ alternatives |
|---|---|
|
Asafetida (heeng)
|
Either buy pure asafetida rock and powder it carefully or buy gluten-free labeled packs (gluten free packs use corn flour or sorghum instead of wheat flour for dilution). If any food is consumed outside, patient/must avoid anything with asafetida. |
|
Other spices (Spices are often ground in machines that also grind wheat, hence are often contaminated with gluten...and this is not expected to be mentioned in "ingredients") |
Either buy solid spices (e.g., solid turmeric, dry chilies etc.) and grind at home carefully or buy labelled gluten-free spices |
|
Vinegar
|
Use distilled vinegar, Apple cider/ cider vinegar/ grape vinegar these are gluten-free |
|
Sauces |
|
|
Gravies, marinades
|
Avoid consuming such food items from outside |
|
Seasonings
|
Avoid consuming/using these |
|
Packaged soups |
Avoid consuming these |
|
Baking powder |
Use labelled gluten-free brand (they use corn flour instead of wheat flour) |
|
Salad dressing, non-dairy creamer
|
Avoid consuming/ using these |
|
Brewer's yeast |
Some brands of brewer's yeast created using sugar beets and are gluten-free. Baker’s yeast and active dry yeast are gluten free |
|
Frozen products |
Avoid consuming these |
|
Toffees, candies, chocolates and even cough lozenges
|
Gluten-free brands of toffee/ chocolates are available |
|
Food colours (especially caramel colour), some
food additives and flavouring agents
|
Only certified gluten free products should be used |
|
Commercially available sweets |
Only home-made sweets with gluten free ingredients in gluten free environment or certified gluten-free sweets can be used. |
|
Commercially available ice creams
|
Only home-made ice creams with no such ingredient or certified gluten free product is to be used. |
|
Some lip balms, lipsticks, certain cosmetics
|
Alternative products with no such ingredient need to be used |
|
Play doh (clay) and some other art supplies
|
Due caution is advised while using these things; there are online sources that teach making clay for playing using ingredients like rice flour, coconut oil and baking soda at home. |
Table-2 Some practical examples of scenarios whereby cross contamination of gluten-free food occurs with gluten-containing food.
|
Scenario |
Tips for Prevention |
|---|---|
|
Getting gluten-free grains/ spices milled at same grinder that mills wheat also |
The grinder/chakki used for gluten free grains/spices needs to be dedicated for these only. |
|
Storing gluten free flour and other ingredients in the containers that are contaminated with gluten |
Using new/ scrupulously cleaned containers for storing gluten-free ingredients |
|
Contamination in refrigerator: gluten-containing food can drop in the bowl storing gluten free food |
Having a separate refrigerator or dedicating upper-most rack of the refrigerator for gluten free food and lower ones for others. The refrigerator must be cleaned scrupulously before starting to store gluten-free food |
|
Wheat dough or other gluten-containing material sticking to ones hands/ cooking slab while cooking gluten free food 
|
Preparing gluten-free food before cooking other items; thorough washing of hands and scrupulous cleaning of cooking area |
|
Cooking pan/ tawa/ chakla/ belan (rolling pin) that is contaminated with gluten 
|
Preferably separate equipment should be there for gluten-free food; otherwise, scrupulous cleaning (extremely difficult!) and cooking gluten-free food prior to the other food |
|
Frying in same oil in which some gluten-containing food was fried |
Fresh oil to be used for gluten-free diet; if oil needs to be re-used, first fry gluten-free food |
|
Air-borne gluten where gluten-free food is being cooked can also be harmful. Whenever wheat roti is cooked, the dry wheat flour is suspended in air...it can enter the gluten-free food and compromise it. |
Gluten-free food is to be cooked first. The dry flour used for cooking can be of gluten-free flour even for making wheat rotis. |
|
Microwave/ toaster etc. can be contaminated with gluten |
It is preferable to have a separate/ dedicated toaster; Gluten-free food is to be cooked first; scrupulous cleaning |
|
Butter/ jam/ ghee contaminated with gluten: If butter/ jam is applied on wheat/ white bread and then from the same container, the jam/ butter is used to apply on gluten-free bread, it won’t remain gluten-free |
Jam/ butter should be dedicated for the celiac disease patient. |
|
Use of salt/ spices from "open containers" while cooking food: The open containers of salt/ spices can be contaminated due to air-borne gluten or with hands while cooking gluten-containing food |
"Sprinklers" should be used as far as possible to avoid cross- contamination |
|
Uncovered gluten-free food lying in the cooking space where other food is being cooked can easily get contaminated |
Due caution is essential to prevent such cross contamination |
|
Contaminated utensils (knife, spoon, chopping board, serving spoon etc.) used while cooking/ serving food. For example, if the knife used on a regular bread is used to cut gluten-free bread, latter won’t remain gluten-free! |
Thorough washing before and after use is essential; even soap and sponge used to wash utensils need to be separate for the utensils of celiac patient. |
Thus, it is clear that maintaining a gluten-free status requires much more than just avoiding wheat and barley as staple food. It requires significant effort on the part of the patient and the family to adopt the changes in procuring, cooking and consuming food: the basic necessity of life. At the same time, it requires tremendous efforts on the part of the treating clinician to convince, counsel and support on a continuing basis to achieve the desired results. Trouble-shooting when the patient is not doing well clinically despite being apparently motivated and compliant is equally troublesome for the clinician!!! However, surmounting big challenges is what gives unparalleled satisfaction, isn’t it?
- Dr. Puneet Kumar, Owner-Consultant, Kumar Child Clinic, S-19, Pankaj Central Plaza, Pocket 5, Sector 12, KM Chowk, Dwarka, New Delhi-110078. www.KumarChildclinic.com
References
1. Gilissen LJWJ, van der Meer IM, Smulders MJM. Why Oats Are Safe and Healthy for Celiac Disease Patients. Med Sci (Basel). 2016; 4(4):21.
2. de Souza MC, Deschênes ME, Laurencelle S, Godet P, Roy CC, Djilali-Saiah I. Pure Oats as Part of the Canadian Gluten-Free Diet in Celiac Disease: The Need to Revisit the Issue. Can J Gastroenterol Hepatol. 2016; 2016: 1576360.
3. Hernando A, Muiico Jr, Mena MC, et al. Measurement of wheat gluten and barley hordeins in contaminated oats from Europe, the United States and Canada by Sandwich R5 ELISA. Eur J Gastroenterol hepatol, 2008; 20(6):545-54.
4. Fritz RD, Chen Y. Oat safety for celiac disease patients: theoretical analysis correlates adverse symptoms in clinical studies to contaminated study oats. Nutrition Research, 2018; 60: 54-67.
5. Position Statement: Oats and gluten-free diet. Coeliac Australia: November 2015 Accessed online on January 4, 2019. https://www.coeliac.org.au/uploads/65701/ufiles/Position_Statements/CAPSOats.pdf
6. Vohra P. What is "Gluten-free" food and Gluten-free cooking In: Celiac Disease, first edition, 2016. National Book Trust: 66-97.

