COVER STORY
VACCINE HESITANCY:
Why is there an uproar?

The view from here:
"One of the dangers of the internet is that we're only hearing like voices, and that makes us more polarized. What's incredible about the net is we have this opportunity to hear more voices than ever. But the tools we tend to build to it have us listening to the same voices again and again." -- Ethan Zuckerman
Last month, I got a call from Mr PC Haldar, former director of Intelligence Bureau (IB) and current president of an NGO in Delhi for an informal chat in his office. I wondered what he wanted to discuss with a clinician! And that too, with one who is settled in a private sector! On meeting him, I realized that he was concerned by the happenings in the vaccine sector. Probably, he wanted to understand the nitty-gritty of this sector and the recent developments including vaccine policies, financing, decisions and lobbying, philanthropists approaches, judicial activism against certain MoHFW's decisions, and the different lobbies active in the field including those actively involved in so-called 'anti-vaxxers' movement, and perhaps, this from an 'outsider', to have an overview of the various issues assailing this sector. The meeting also changed my earlier perceptions regarding IB. Everybody thinks that this organization has only to deal with insurgency, security threats from outside and inside the nation, nabbing terrorists, etc. During the discussion, I came to know the exact scope of functioning of this agency which was far more broad-based than being confined to the security and internal strife. It was only during the early 90s' that the functioning of this establishment came to light during J&K conflicts. I was surprized to know that prior to the 90s', the agency used to perform certain tasks that were not even distantly connected to the nation's security like investigating underlying factors behind the rise in daily commodity prices, black-marketing, scarcity of daily consumable products, etc. So, the agency's role was not merely confined to safeguard the nation's security but also to ensure socio-economic well-being.
This experience was an eye-opener to me. Issues pertaining to vaccines and vaccination practices are not bothering public health professionals only, but even non-health experts and professionals are also getting increasingly concerned about them. 'Vaccine hesitancy (VH)' is one such issue that's creating lots of news in both health and non-health sectors. The WHO has recently ranked it as one of the top 10 health threats in the world for 2019. The whole western world, mainly the Europe and the US, is in the grip of this alarming threat that has the potential to neutralize all the gains made over decades by vaccination all over the globe. Confidence in vaccines is an increasingly important issue for global public health. Lack of credibility is a well-documented cause of outbreaks, delays and setbacks for global polio eradication, as well as difficulties for the achievement of other goals of immunization. So, it is understandable to see the huge attention being paid by the governments, health agencies and philanthropists on this matter.
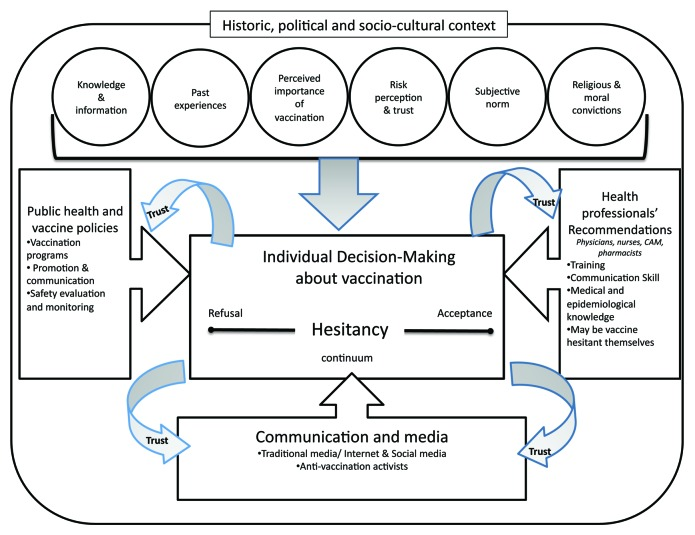
Figure 1 : The interplay of Vaccine hesitancy, communication, decision making about vaccination, and public health vaccine policies.
Is 'hesitancy' the right term?
The growing influence of anti-vaccine lobby in the West forced international health agencies, including the WHO, to reinvigorate its efforts to take this menace head-on with the formulation of a new front under new terminology. The WHO-SAGE Working Group from 2012-2014 toiled hard to come out with a perfect term that could categorize factors that influence the behavioural decision to accept a vaccine, and in 2014 they agreed upon 'Vaccine hesitancy (VH)' as an ideal term to describe different issues related to the implementation of vaccination drives in a community (Figure 1). There was some debate on whether 'hesitancy' was the most appropriate word to describe these issues. Concerns were raised that 'hesitancy' had a negative connotation. Another term that came under consideration was 'vaccine confidence', a more positive word. While 'confidence' covers a range of issues such as trust in vaccines, trust in health-care workers delivering the vaccine and in those making the decisions on approval of vaccines for a population, yet the word 'confidence' still seemed narrow in scope as if covering only one category of factors that affect vaccination acceptance decisions. Although the exact meaning of VH is the 'pause' people take before deciding to go for a particular vaccine or not, the WHO believed that it encompasses broad sentiments of the community about vaccines and vaccination, and include a variety of terms like vaccine confidence, vaccine trust, vaccine safety, misinformation about vaccines, vaccine acceptance, vaccine resistance and refusals, antivaccine movements and anti-vaxxers, vaccine demand, etc. At one end of the spectrum are those who willingly accept all the vaccines, and at another extreme are those who refuse all.
The high rate of childhood vaccination coverage in most countries indicates that vaccination remains a widely accepted public health measure. However, these national estimates may hide clusters of under-vaccinated individuals. Many recent outbreaks of vaccine-preventable diseases (VPDs) have been linked to under-vaccinated or non-vaccinated communities (Box 1).
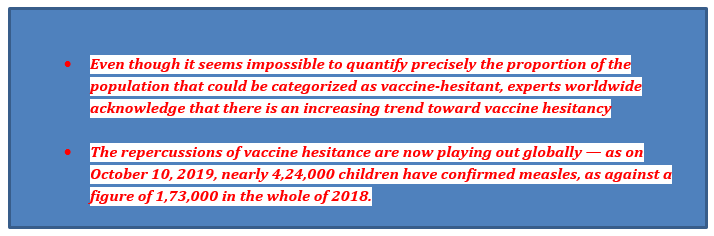
BOX 1 : Prevalence and impact of Vaccine Hesitancy.
Epidemiology of Vaccine Hesitancy
Vaccine hesitancy is not only context-specific but also varying across place and time. According to a recent publication, low- and middle-income countries (LMICs), in general, had lower rates of VH and, for example, had fewer safety concerns about vaccines compared to high-income countries (HICs). The most hesitant countries were found in eastern Europe, and then in western Europe and northern America. At 95%, people from South Asia trusted vaccines the most followed by eastern Africa at 92%. Western Europe and eastern Europe brought up the rear with just 59% and 52%, respectively.
Is it relevant to us?
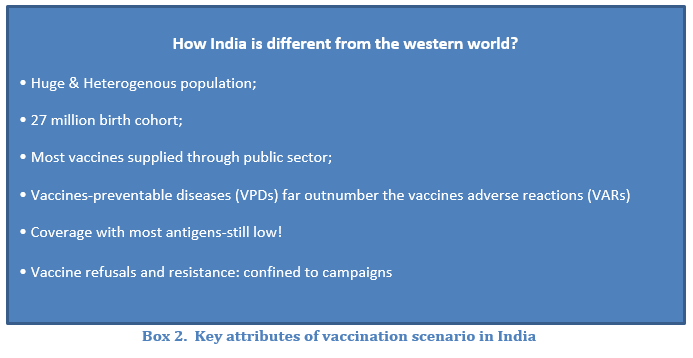
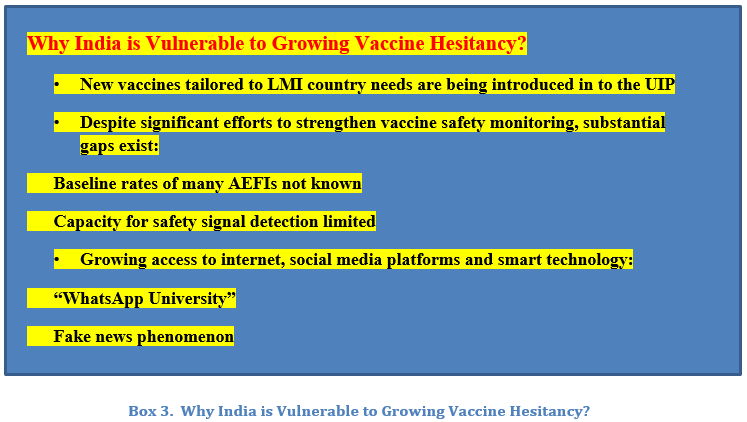
No country is immune to the impact of VH on the vaccination rates against VPDs. And India is no exception. However, the face of VH is a bit different here. What we are encountering is more of misconceptions and misinformation against vaccination drives that result in resistance against vaccination and vaccine refusals. However, even in this scenario, there is a perceptible change. During the polio drives, the dissenting section of the population was the underserved, marginalized, and poorly educated people residing in two large northern states. Whereas during the recent measles-rubella (MR)-campaigns, the section of the society responsible for VH was more affluent, more educated and living in more developed southern states of the country. This was not surprizing given the heterogeneity of our population. Boxes 2 & 3 enumerate the key attributes of Indian vaccines scenario and the existing threat of VH to the country.
The changing face of Vaccine Hesitancy in India
Of late, there are a flurry of activities in terms of workshops, seminars, CMEs, etc in India on vaccines safety, confidence and hesitancy and its looming threat on our vaccination scenario and vaccination rates. Is the scenario indeed equally bad here also as it is in the industrialized countries? The VH in India is characterized by rumours, religious edicts, refusals and the resistance. This trend is so far confined to the opposition of large vaccination drive undertaken by the government. The type of VH that is prevalent in the western world where the well-educated and financially well-off parents start doubting the utility and safety of vaccines and consider them as redundant, has not yet manifested overtly here.
Few recent personal experiences have pointed out that even this type of hesitancy does exist and is silently brewing even amidst top professionals. In the first instance, District Magistrate of my city refused to get the Rotavirus vaccine administered to her son despite being a medical graduate herself. Probably she was not convinced about the efficacy of the vaccine. In yet another instance, an HOD of the Microbiology department of a premier institution of the country was sceptical of the practice of giving too many vaccines at a single visit. He feared the practice may lead to overloading of the immune system if too many antigens are administered simultaneously! Another colleague of him, a renowned immunologist of the same institute, believed that the vaccines had some definitive role in the development of autoimmunity. These few instances baffled me since these apprehensions were not based on science and evidence. When your top health professionals are having reservations regarding the well-established and scientifically proven process of vaccination, what can be said about other non-medical professionals! In the west, resisting vaccines has become a vogue. Anti-vaccines sentiments are finding more and more takers there. However, the persistently high burden of many VPDs and the poor-affordability of non-UIP vaccines are the reasons why a true, west-like VH is still not seen here in India. But we need to be vigilant since the omens are not good.
Reasons for Vaccine Hesitancy
The main reason behind the genesis of VH is 'misinformation'. Social media is used in stirring fear in people by falsely blaming vaccines for unrelated diseases is the bedrock of the VH across the globe. Further, anti-vaccine conversations often centre around moral outrage and structural oppression by the government and the media, suggesting a strong logic of "conspiracy-style" beliefs and thinking. Sometimes, people give vent to their dissatisfaction with the civic administration and ruling regime through closing doors on vaccinators and refusing vaccines altogether. As mentioned above, the refusals of polio drops during the height of polio eradication drives in UP and Bihar was due to the misconception that the polio vaccine caused illness, infertility and was ineffective. Religious propaganda and inconvenience in accessing vaccines are other reasons.
Vaccines, the enemy of their own success!
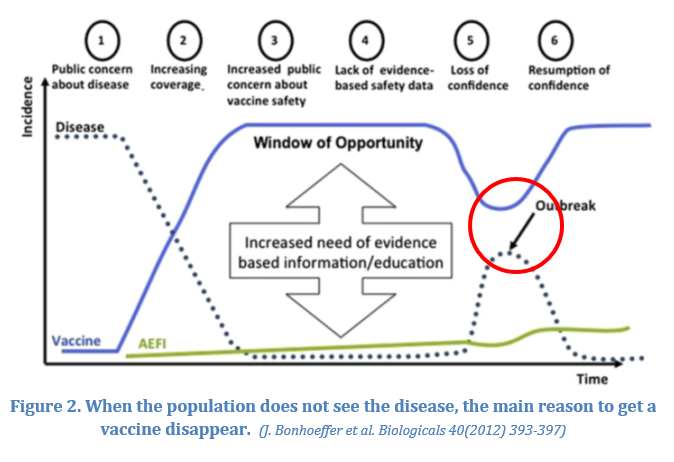
At first sight, this seems quite strange and a bit 'oxymoronic'. Let me explain. Certain vaccines have been so effective that they have eliminated or significantly reduced the burden of the 'wild disease' from a large region of the globe (Figure 2). There are counties where the vaccines-related adverse events have far outnumbered the actual number of VPD against which the vaccine is employed. This scenario is more prevalent in western countries. As a result, there are instances where young clinicians have not seen a particular VPD in their lifetime. I do still remember an anecdote shared by my MD guide, Prof. Kanwal Kalra during her ward rounds in the late 80s. During one of her visits to a reputed pediatric UK hospital, the entire pediatric unit failed to diagnose a classic case of measles - an entity not even considered worthy of a discussion during ward rounds here! The young UK pediatric residents were bewildered on seeing a case of fever with a rash that they had not encountered in their training so far. And they were equally mystified to see the ease with which she had made the spot diagnosis of the case! But now the scene has reversed. The entire US and many European countries are in the midst of huge outbreaks of measles, a disease they had so efficiently eliminated two decades back! And this was all due to this phenomenon called VH. People of these countries are now more scared of vaccines than the diseases the vaccines prevent. Hopefully, this resurgence of an old, eliminated VPD may reinstate their confidence in vaccines.(Figure 2)
The menace of internet and social media
Traditionally, the vaccination scenario is monitored with surveillance of VPDs, monitoring vaccine coverage, and surveillance of 'adverse events following immunization' (AEFI). But in 2020, the scenario has changed. It is not enough to maintain and monitor only these traditional databases. The game changed perhaps between 2010 and 2012. There was a bombardment of information transmission and exchange at digital platforms, mainly on social media. Hence, monitoring of the digital world has now become an integral component of new frontiers in vaccine safety intelligence and to safeguard against frequent disruptions of vaccination drives.

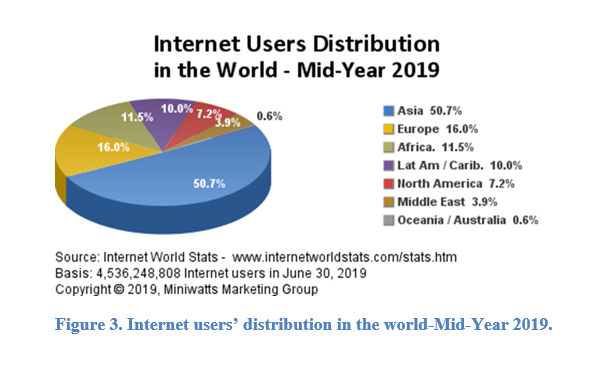
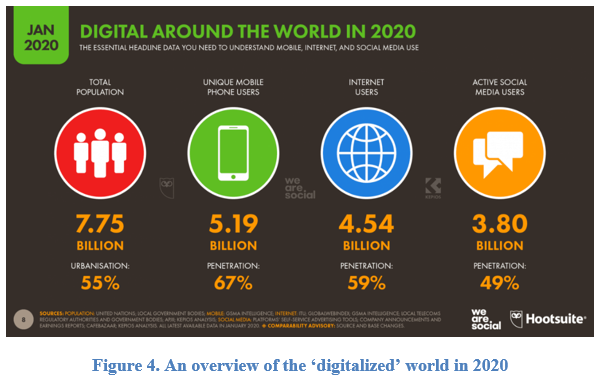
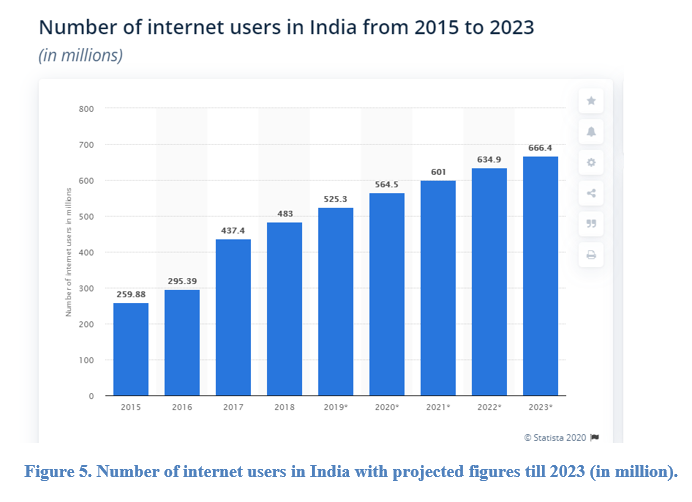
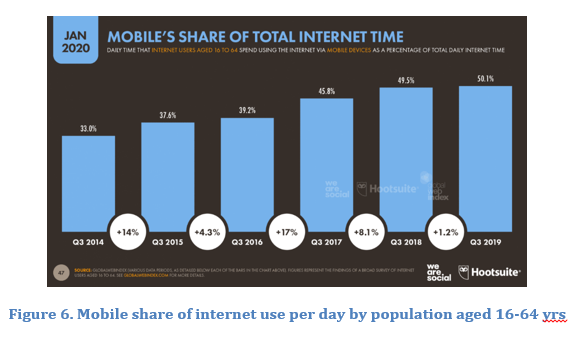
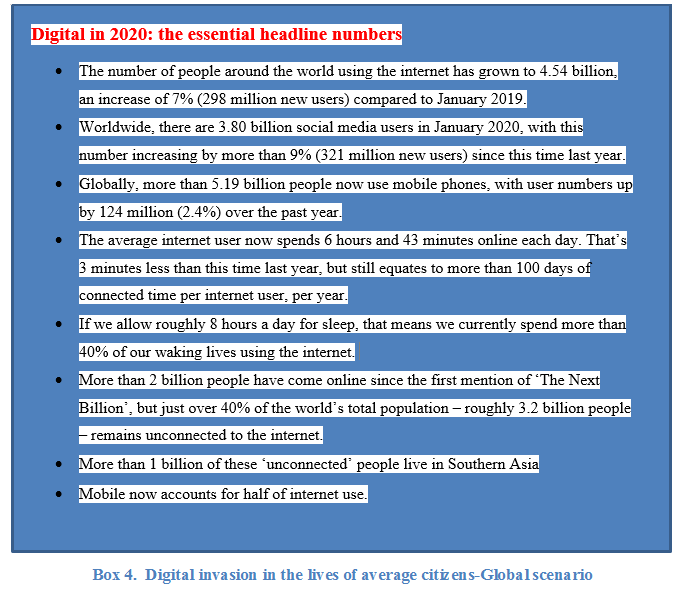
The role of digital world has reached new heights in our lives, with more people spending more time doing more things online than ever before (Figures 3-6, Box 4). With the advent of social networking platforms like WhatsApp, Facebook, Twitter, Instagram, Tik-Tok, etc, the anti-vaccine movements gained momentum. While Twitter is far more popular in many European countries and the US, in India it is the WhatsApp that is at the forefront of driving most of the misinformation campaigns and fake news on vaccines. Research suggests that the anti-vaccine movements on social media 'echo-chambers' is enormous and dangerous.
Vaccine refusal has also been promoted on social media. A study found that Twitter users who were more often exposed to negative opinions about the safety and utility of human papillomavirus (HPV) vaccines were more likely to tweet negative opinions than users who were more often exposed to neutral or positive information. These tweets, which included misinformation, anecdotes, and opinions that may result in vaccine hesitancy or refusal, made up most HPV vaccine-related information exposures for nearly 30% of users that tweeted about HPV vaccines during the study period. Besides, users expressing negative opinions about HPV vaccines were more closely connected to other users expressing the same opinions.
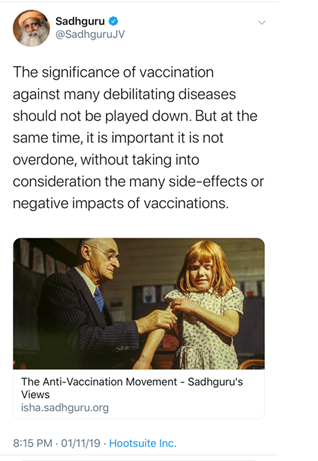
Another recent example is the a comment made by Jaggi Sadhguru through his official twitter handle. While acknowledging the contribution of vaccines in tackling many debilitating infectious diseases, he commented on the 'negative' 'side-effects' of vaccinations, particularly when 'overdone'! This will give 'anti-vaxxers' the much-needed spur to scare parents from vaccinating their children.
The above tweet by Sadhguru has a link to an article published on the Isha website on October 3, which is an excerpt of a conversation between Jaggi Vasudev and Dr Soumya Swaminathan (Chief Scientist at WHO) that was held at the UN General Assembly on June 27, 2019. (The article also has a link to the taped conversation, on YouTube.)
During the conversation with Dr Swaminathan, he is seen advocating vaccination and spelling out the gains India made by preventing children from becoming crippled through oral polio vaccination. But soon he veers off track and ends up spreading dangerous misinformation about influenza (commonly referred to as flu).
With a disclaimer that he is not a medical expert, Jaggi Vasudev says: "…From listening to parents [in California], this is what I gathered. I thought some of the things they were giving vaccines for were just absurd. If a child catches a flu or something like this, it is all right to go through some of these illnesses when you are growing up."
This might turn out to be an irresponsible statement to have ever been said from the hallowed platform of the UN. Unfortunately, the patently wrong message went unchallenged, giving it a ring of truth. The incorrect messaging did not stop there; it is now posted on the Isha website, increasing the chances of more people being misled. The blithe comment about flu sans any evidence is in stark contrast to the seriousness with which WHO and the CDC treat it. Its repercussions can be lethal to the society struggling hard to shrug off the challenge posed by a new, ongoing devastating pandemic of COVID19!
Analysing the Microcosm-the behaviour exploration
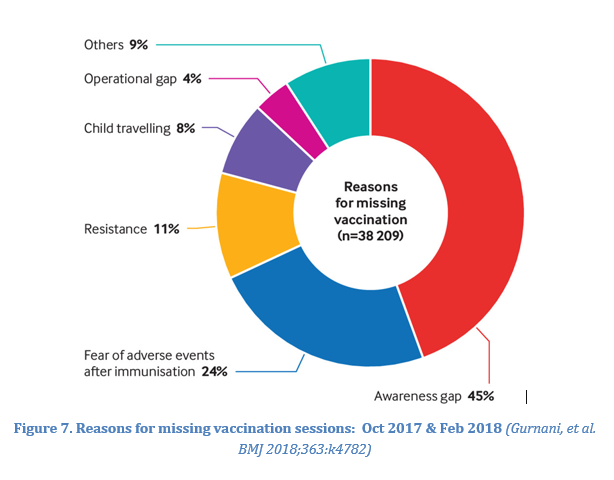
What causes people to doubt the utility or to refuse the intervention that's protective to their progeny and ensures long survival of them? As explained above, the lack of awareness, misconceptions, fear of adverse events, lack of affordability, poor infrastructure to deliver vaccines, lack of faith in government, political biases, etc are the reasons for low uptake of vaccines and resultantly low coverage in India(Figure 7). They are understandable to some extent given the overall socio-economic milieu of our population. But why the people in the affluent countries have doubts about the motive and the process of vaccination? Why suddenly the 'anti-vaccines' movements have started gaining momentum? Many public health experts those in charge of large vaccination drives, and behavioural scientists have started analysing the social nature of vaccine decision-making.
After analysing in detail for many years, they have a good understanding of the reasons why parents reject vaccines and the aspects of vaccines that they fear the most. The most 'vaccine deniers' distrust the expert systems which design and deliver vaccines and that they regard the vaccines as an 'unwelcome' and 'unnatural intrusion' into a 'natural body' which they view as unneeded or unbeneficial.
Now we know that the vaccination behaviours of our social networks are a predictor of our behaviours, so our milieu matters to the decisions we make. And, here comes the roles of 'homophily' and 'influence'(Figure 8). Homophily refers to humans' tendency to associate and connect with individuals similar to them in certain aspects, people who share their interests, values, culture, who have the same demographical, racial characteristics, etc., which leads to one of the main characteristics of a social network, which is homogeneity. This principle of homophily is the foundation of the most various human relations and networks, from marriage, to friendship, work, information exchange, and others. Homophily limits people's social worlds in a way that has powerful implications for the information they receive, the attitudes they form, and the interactions they experience. The behaviour of people online seems to be following an intrinsically human principle of behaviour that guides our actions in real life.
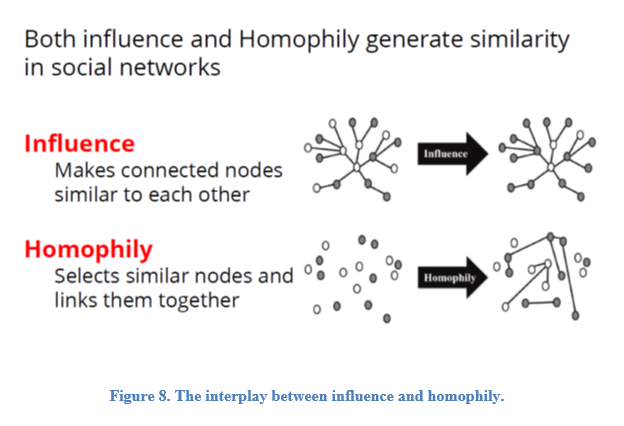
'Homophily': Birds of a feather flock together: Homophily, a concept that can be expressed by the saying: birds of a feather flock together, plays an essential role in shaping our individual and collective view of the world. One example is online social network platforms like Facebook. Facebook today is the most populated country on earth that too without geographical boundaries! As of the third quarter of 2019, it has 2.45 billion monthly active users. People connect with other individuals that they know in real life, and with whom they have common interests or other socio-demographical, behavioural, and intrapersonal characteristics, and then with the friends of their friends, and with potential friends that are automatically suggested to them by these applications, based on common profile characteristics.
But, as Zuckerman-an expert on behavioural science, exclaims "Homophily can make you really, really dumb". This exclamation is not too far from the fact. Though we efficiently and "comfortably" communicate with like-minded individuals on the social networking sites and other digital platforms, we tend to avoid contacts that take us out of our "comfort" zone, which can be a field that we are not in control of, have few information about, or are unaware of: "We know so little about one another, and what we do know is generally so wrong, that our first instinct is to try to shut each other off. Fighting the homophily instinct is an effort that will lead us to the better or full use of technology.
There is another term more frequently used in context with VH, the 'Social media echo chambers'-where users only hear and see the information that echoes their own beliefs. This further energizes the anti-vaccine movement.
The homophily concept sums up nicely the formation of many anti-vaxxer groups online and on social media. It is not the digital world and the internet that is intrinsically wrong, but that people tend to use it in limitative ways: searching and selecting information and individuals mainly to reinforce their own ideas, which are sometimes not based on the scientifically proven facts. This is what is happening in the affluent society of developed countries.
What is missing is a theoretical account of how and why this is the case; how the beliefs of vaccine-hesitant or rejecting parents are socially constructed, acquired and reinforced.
Does religion have something to do with VH rates?
Religious propaganda that the vaccine may contain microbes, chemicals and animal-derived products which are forbidden by religious laws have a major impact in certain communities. Although in certain countries particular religious groups were more vaccine-sceptical than other groups, no one religion was globally predictive of negative attitudes. This indicates that the effect of faith on vaccine attitudes is dependent on the local context and that these attitudes are not necessarily driven by religious doctrine in itself, but mediated by political, socio-cultural and other factors.
However, some religious groups like Muslims were associated with lower vaccine coverage in several sub-Saharan African countries, both for boys and girls. Hesitation and resistance to vaccination is a substantial issue in some districts of Kerala, India. In the Malappuram district of Kerala, which has a substantial Muslim population, it was found that factors such as religion have only a minor role in resistance to vaccination. On the other hand, many religious leaders openly support vaccination drives and consider that religious texts and beliefs do not oppose disease prevention.
The 'antivaccine lobby' and 'anti-vaxxers'
Another issue hurting vaccines and control of VPDs is growing antivaccine lobby and anti-vaxxers. The anti-vaccination sentiment is as old as vaccination itself. And the fact is that anti-vaccination movements are unlikely to disappear soon. While a minority of parents hold strong anti-vaccination sentiment, the proportion categorized as vaccine-hesitant may be increasing; even parents who vaccinate their child can have important doubts and fears regarding immunization. With the Internet, the anti-vaccination movements are becoming more powerful than ever and have the potential to reach and influence many parents. There are several anonymous anti-vaccination messages on social media that have no clear sources other than blogs and dubious publications. A lot of these websites are still referencing Andrew Wakefield's retracted and fraudulent paper published in 'The Lancet'. Compare this with the real doctors and healthcare professionals and experienced scientists who are willing to put their names and list their experience and qualifications on messages that support vaccination. Despite significant efforts, few, if any, public health strategies have effectively and long-lastingly succeeded in countering anti-vaccination movements.
How to counter Vaccine Hesitancy?
Now it is time to take VH head-on. It is time to move beyond the 'knowledge deficit model' and to develop innovative responses to address anti-vaccination sentiment. The first and important step to develop effective strategies is to have a good understanding of both the causes and the contexts leading to vaccine hesitancy and refusal. Interventions must be tailored to address the specific concerns in each context.
The methods employed to deal with vaccine misinformation and refusals until quite recently may not be effective in today's time. The world has moved forward and become a large playground without any boundaries. The walls and roofs are demolished by the onslaught of digital media. New digital platforms have unleashed innovative practices that enable novel forms of communication and greater global reach than at any point in human history. But on the other hand, disinformation and hoaxes that are popularly referred to as "fake news" are accelerating and affecting the way individuals interpret any new development. And vaccines are no exception. Fake news and sophisticated disinformation campaigns are especially problematic, and there is a growing debate on how to address these issues without undermining the benefits of digital media.
Our communication strategy to deal with disinformation and fake news should be reliable, trustworthy, timely, adapting to the context of the discussion, tailored to the needs, easy to understand, engaging, and interactive. At the same time, we must undertake some innovative projects like monitoring of social media portals using web analytics to effectively deal with 'web invasion' by anti-vaxxers and anti-vaccine lobby. There should be a provision of dealing with any vaccine safety concern with 'real-time' intervention by the nodal agency during an ongoing immunization campaign/drive. Do we provide all that?
It is heartening to see that people are giving more importance to understanding behavioural science behind vaccine acceptance and developing an 'evidence-based communication strategy' to deal with growing VH rates, especially in the western world. Many studies have shown that parental decisions to use or avoid immunization for their children are complex and multi-dimensional, including contextual determinants, determinants related to the vaccination services and individual determinants, such as parents' knowledge, attitudes and beliefs or sociodemographic characteristics.
The growing interest in vaccine hesitancy has resulted in the development of different tools and strategies to enhance vaccination acceptance. Many experts have proposed ways to counter vaccine hesitancy at the population level, including transparency in policy-making decisions regarding vaccination programs, providing education and information to the public and health providers about the rigorous process that leads to approval of new vaccines and diversified post-marketing surveillance of vaccine-related events. Additional emphasis should be placed on listening to the concerns and understanding the perceptions of the public to inform risk communication and to incorporate public perspectives in planning vaccine policies and programmes.
How to manage social media?
As stated above, the greatest threat to vaccines and vaccination projects is from the antivaccination movements run through social media. Monitoring of social media is one option though it may have some implication on individual privacy rights. Web-analytics is another novel intervention. But can we monitor and pre-emptively disrupt any growing negative vaccine sentiment build-up that may result in outbreaks of VH (mass refusals) during a campaign by using this technology? We need to ponder over this. At the same time, there should be regular beaming of pro-vaccine information and vaccine-success stories through various social media engines.
Conclusions
Vaccination is a great success, but we need to stay vigilant. Vaccine hesitancy is a real and greatest threat to vaccination programs. It does exist in India; so far, confined to public vaccination programs, but the incidence of VH is increasing among individuals in both high and low socioeconomic strata. Social media, particularly WhatsApp is the major driver, particularly in India. We need to keep a high vigil to avoid disruption of vaccination activities and at the same time, need a new intervention strategy with a focus on social media. There is a need to understand the social behaviour of the community, and to develop a multidisciplinary approach to tackle growing anti-vaccine movement.
-Vipin M. Vashishtha

