The view from here:
"A doctor will be close to 40 years of age when he becomes a specialist or super-specialist. From there it takes a decade more of hard work day and night, Sundays and holidays, to get recognised. No other profession has such a long incubation period".
- J.S.N. Murthy in The Hindu
Don't convert doctor into an endangered species!

Vipin M. Vashishtha
After a hectic busy OPD, an apneic, listless, pale child was brought to my clinic. As I approached to examine the child, somewhere in my thoughts, I was 'fearing' the prospects of finding few heart beats and the subsequent process of reviving and then ventilating the child. The consequences of facing the wrath of the relatives in case of an unfavourable outcome were indeed very scary and frightening. After thoroughly auscultating for few minutes and not finding any cardiac activity, I took a sigh of relief and 'conveniently' declared the child as 'BD', i.e. brought dead.
Now, on reconsidering the whole scenario taking place 25 years back when I had just started my clinical practice, I would have been looking for those 'elusive' beats at that time too, but the intent to revive the baby would have been intense and without fear. Then I would have wanted to salvage the child by whatever means available. And not finding any beat would have thoroughly dejected me. Since I wanted to save the life of my patient which was, and still should be, my motto and ethical posturing. Today, I am more interested in saving myself. From the hassles of undergoing through the utmost mental strain of declaring a child dead after undergoing a long protracted intensive care management that would have caused intensive mental botheration to me and my staff, and would have also incurred huge expenditure to the family. So, I was scared of the scenario where I might have to face the fury of the dissatisfied parents who would have dubbed me as a greedy physician who had subjected them to an unnecessary, unrewarding, prolonged and hugely expensive ordeal.
This is a very apt depiction of 'defensive practice' that has crept in to our profession. I do still remember a recent incident when my efforts to give prolonged CPR to a critical child was seen as an attempt to remove kidneys of the deceased child, and my hospital was ransacked and thrashed! Today, there is a huge trust deficit between doctors and their patients. With the advent of consumer protection act and corporate culture amongst practitioners, the status of a patient has changed to a consumer and the doctor has become a service provider who can be held responsible for any slackness in the service provided. Consequently, the patients their relatives' expectations have also changed. They are not willing to accept any unfavourable outcome. Whatever may be the status/nature of the disease of their patients. They want absolute value for the money spent on the health care of their critically ill patients. Anything less would follow the usual chaos-- the physical assaults on the doctors and their premises and litigations. Today the reputation of the doctors is at nadir.
Who is to be blamed for the current state of affairs? The doctors, their regulators and professional bodies, the society, or the government? I think the blame should be borne by the all . The shortcomings at different levels are responsible for the altered dynamics of patient-doctor relationship in today's time.
The worst year
The 2017 was probably the worst year in the last decade for the entire medical fraternity. Be it assaults on doctors by the patients' relatives, media or the establishments, imposition of draconian 'Clinical Establishment Act' in many states, unfortunate deaths of large number of children owing to administrative lapses, unprecedented government strictures on health sector, or the infamous seizure of crores of stacked cash from the doctors. All these events have somewhat adversely affected the overall image of the doctors and medical profession. And, in the last, the dismantling of MCI and its substitution by the National Medical Commission (NMC) Bill has enraged the whole medical community. The doctors and their associations were forced to undertake the route of agitation, on the roads, in their clinics, and inside the court premises also.

Dismal and uneven state of health
While facilities in Indian metros are competing with the world's best medical centres, the scenario beyond the urban areas is quite pathetic. The demand and supply in healthcare services still show a significant disparity in urban and rural areas as also regional imbalances. For example, 30% of Indians do not have access to primary healthcare facilities, about 39 million Indians fall below the poverty line each year because of healthcare expenses, around 30% of people in rural India do not visit hospitals due to fear of the expenses, about 70% of Indians spend all their income on healthcare and drugs, and 47% of healthcare needs in rural India are financed by loans or the one-off sale of assets. The health infrastructure is heavily skewed in favour of urban areas. Nearly 75% of dispensaries, 60% of hospitals and 80% cent of doctors are located in urban centres. Doctors cater to a third of the urban population, or no more than 442 million people. India has got excellent infrastructure for public health but is entirely non-functioning. PHCs do not exist in many villages (about 1 for every 20 villages), and where present are so acutely undermanned that the "access" system is broken at the first mile. As many as 18% of PHCs are entirely without doctors. Our healthcare facilities have grown significantly in terms of numbers and expertise of our professionals, but this has largely been in the private sector. The government's failure to deliver quality care has led to a rapid expansion of private hospitals, which today account for 93% of all hospitals (up from 8% in 1947), 64% of all beds, and 80- 85% of all doctors.
Scarcity of doctors
There is huge shortage of trained doctors in India. In my own district, the Government run District Hospital does not have a general or orthopedic surgeon for last 6 months. There is no cardiologist nor a CT Scan machine in the entire district which caters to more than 3.5 million population! More than 60% of the doctors' post are lying vacant owing to unavailability of doctors.
Let's have a look on the status of trained health care professionals in the country. Nearly 30,000 doctors, 20,000 dentists and 45,000 nurses graduate from medical colleges across India every year. However, the doctor-to-patient ratio in India is only six for every 10,000 people or one doctor for 1,700 people, compared to the WHO norm of 1:1,000. Most of these doctors are in urban regions, while close to 70% of Indians live in rural provinces. This is far below the rate in Australia (1 for every 249), the US (9 for every 548), and the UK (5 for every 1,665). The global ratio stands at 15 doctors for every 10,000 people. Further, the distribution of doctors is also uneven across the country, with a low ratio in states like Chhattisgarh and Jharkhand-just two doctors for every 100,000 people. And there are only six hospital beds and two surgeons per 100,000 population. Out of 50,000 UGs produced every year we have only 15,000 PG seats and for general category only 8000 in a country with 1.2 billion population! This gap isn't going to close any time soon. A 2015 Parliamentary Standing Committee report mentioned that even if India were to add 100 medical colleges per year for five years, it would take till 2029 to achieve the WHO prescribed ratio.
These figures on the shortage of trained medical professionals in India are shocking. But even more shocking is the government's and the society's attitude toward doctors. And media is not far behind. The way the government and other establishments are targeting doctors, they would become extinct in near future! Already, barring from the children of the doctors who have their own setups, most of the students are shying away from medicine as a future career option. There is a perceptible decline in the number of students opting for biology after 10th standard across the country. Yet, the witch-hunting continues.
The government's apathy
It is well established that health is not a priority for the governments or any political outfit. And current government is not an exception. Nobody wants to talk about the elephant in the room. It is indeed baffling to know that while 'swatch bharat abhiyaan' is a flagship program of the present central government, no significant impetus is provided to public health which is directly linked to cleanliness. How can one disengage health from the cleanliness? Still the budgetary allocation to health is a meagre 1.3% of entire GDP, well below the global average of 5.99% though it has promised to increase public health spending to 2.5% of GDP in a time-bound manner. Many neighbouring countries are spending much more on health than us (Figure 1). No wonder, with this much spending on health, India ranks "close to bottom of the pile" on most international health indices. India ranks 180th out of 192 countries in the whole world in government spending on healthcare for its own citizens! Compared to its spending on health, India spends around 2.4% of its GDP on defence. Global evidence shows that, unless a country spends at least 5-6% of its GDP on health with most of that coming from public funds, basic healthcare needs are unlikely to be met. This is a travesty of social justice, and all governments including the present one have hidden this squalid fact so the public never know what government can and should do. Quite astutely, the government is seen passing the buck to the hapless doctors on their poor performance in heath arena. They are seen joining the society in doctor bashing without discharging their fundamental duty of providing health to every citizen of this country.
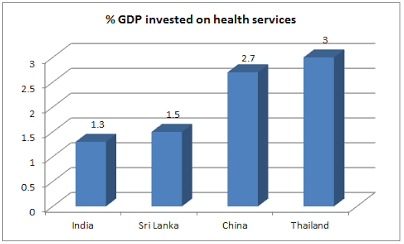
Figure 1. Public spending on health (% of total GDP) by some neighbouring countries
The role of doctors, professional bodies and industry
Today there is no empathy and respect for the doctors in the society. Even any charitable act by them is also viewed with cynicism and suspicion. Doctors, their professional bodies, and their regulators are also equally responsible for the current state of affairs! Few black sheep have destroyed the respect of the doctors they quite earnestly deserve in the society. Let's stop trouncing Vivek Bindras , we have plenty of Ketan Desais and Rajeev Guptas in our midst! We have shed ethics, morality, honesty, compassion, and many other humanitarian values long before. And now we expect the society to give us the same respect that we enjoyed decades back! The advent of corporate culture in to the medical field has scrapped away whatever little veil of patient- welfare existed. They have brought stark consumerism and entrepreneurship in to a noble profession, and converted doctors to their sales executives. The recent headlines related to few incidents in the big corporate hospitals are the fallouts of this very trend.
What about the professional bodies and regulatory authorities of the doctors? The less said is better. The MCI was the epitome of corruption. It has outlived its utility. It has failed miserably in instilling reforms in medical education rather it has institutionalize the corruption in it. On the front of protecting medical ethics and preventing malpractice, it has become a redundant, toothless organization. So it ought to have scrapped, sooner or later. We should not mourn its demise. In last few years, the MCI has become literally a prisoner of Ketan Desai and his gang. And, what the IMA, the largest association of doctors in the country having more than 2.75 lacs members, did is equally deplorable. They have not only approved the functioning of Ketan Desai but even felicitated him by starting an oration in his name at the 78th IMA Central Council Meeting!
Add to all these happenings the unethical marketing practices of industry and their unholy nexus with the health care professionals. Corruption is the root cause of many ills prevalent in the health sector today. Be it private or public. Right from the medical education to individual practice to large public health interventions. The things have reached to a level when the pharma companies arrange huge sum of money used as a bribe to buy a CMO post of a district. The prospective candidate for the post merely needs to give his/her consent to the future auctions and the 'loot' by that pharma company. In fact, they auction a CMO post to the 'highest bidder' in the upcoming game of corruption!
The NMC bill
There may be some merits in the proposed NMC bill like providing minimum basic knowledge to Ayush doctors serving at the remotest areas of the country. As described above, there is an extreme shortage of doctors particularly in the remote rural areas. There are instances where a pharmacist is seen performing surgery and a sweeper is dispensing medicines at a public health picket. At most interior places, quacks are the first point of contact for the most rural folks during the time of emergency. So, the immediate need of the hour is to train these delivery points in the basic health care course of short duration till we have adequate trained doctors to man these interior health centers. The IMA is vehemently opposing the proposed provision of 'bridge course' in the NMC bill fearing that the move will result in unscientific 'mixing' of different systems of medicine and Ayush doctors would be treated at par with a MBBS doctors! I think, we are probably over-reacting to a non-issue. The intent seems to be good but inappropriately worded that is the root cause of disquiet and anger amongst the allopathic doctors. The designation of 'bridge course' seems to be a misnomer lest the central government and MoH do not have any hidden agenda or any sinister intent of undermining the virtues of modern medical training and practice. The NMC bill has provision for four autonomous boards, one each to oversee UG education, PG education, accreditation, and ethics and registration. If all these proposed bodies work earnestly, many ills associated with the MCI can be taken care of even if they are governed by the non-medicos. The MCI fostered corruption with a coterie of people running all the activities. This arrangement resulted in a scenario where in the 'regulated' electing 'regulators'! Even the provision of 'exit test' makes sense as this would shift the focus from infrastructure and personnel to the quality of education. The private medical institutions should be graded based on the quality of education they are providing to their students, not merely by the infrastructure, facilities, teaching faculty, etc. High failure rates in the exit examination at a given institution would signal its poor quality of education to potential applicants.
What is needed?
Health is a fundamental right of every citizen. Failure to provide health would have legal consequences. The first and foremost thing to do is to accord a high priority to health and health sector. The government must at least double the expenditure on health from its existing allocation. The public health delivery system especially in the rural areas should be bolstered by creating adequate delivery points. The existing delivery points including quacks should be brought in to the fold by imparting basic training courses in emergency healthcare. When even sub-Saharan African countries can successfully address the problem of shortage of doctors by training non-doctors in basic health care, why cannot we apply the similar model here! The scarcity of MBBS doctors in the country should be another top priority for the government. Efforts should be made to double the existing UG and PG seats. The existing district hospitals at every district headquarter should be upgraded and converted in to a medical college. Till adequate MBBS doctors are available, other innovative options like creating cadres of 'rural doctors', training of Ayush doctors in delivering basic minimal healthcare, limited privatization of rural healthcare delivery, etc can be thought off. Many shortcomings of the upcoming NMC Bill must be corrected at the earliest to make it a truly 'game-changing' reform. It must be made free from political clutches. It is a known fact that many private medical establishments are run by the politicians especially in western and southern India. It is high time, the government should speed up the much needed reforms in the health sector with setting up of rigid timelines. Apart from rebuilding the primary healthcare, there is an urgent need to strengthen medical insurance coverage in the country to make quality healthcare affordable.
The government ought to take health care professionals also in to confidence to implement these changes at different levels. The grievances of today's health professionals need to be addressed. The government should resist the temptation of bringing extreme bureaucratic control with the new health Bill and introducing coercive policies at ground level. We, the doctors, should also mend our ways. We need to cooperate with the establishment on certain welfare-oriented schemes of the government. We also need to set our houses (bodies) in order keeping the long forgotten old values upfront. At the same time, the government should also need to deal the doctors with care and compassion lest they may turn in to an endangered species. J.S.N. Murthy also echoes the same sentiments, "every doctor is doing his or her best for the patient. Don't shoot the doctor; he or she is helpless. It cannot happen to lawyers, bureaucrats, industrialists or politicians because there will be repercussions"!
BOTTOMLINE:
"It is for society to profit from medical science -- it is not for medical science to profiteer from society!"
-Ram Nath Kovind, Hon'ble President of India
Key references
- Village Diary of a Heretic Banker Paperback - June 6, 2014 by Moin Qazi (Author)
- http://www.thehindu.com/opinion/open-page/why-blame-the-doctor-for-the-ills-of-the-system/article21381819.ece
- https://www.counterview.net/2017/12/with-mere-13-of-investment-of-gdp-india.html
- http://www.thehindu.com/opinion/op-ed/prescription-for-the-future/article22413556.ece
- https://blogs.timesofindia.indiatimes.com/toi-edit-page/threshold-of-renaissance-medical-education-is-in-desperate-need-of-transformation-nmc-bill-can-bring-it-about/?utm_source=Mailer&utm_medium=ET_batch&utm_campaign=ethealth_news_2018-01-11

