Spotlight
Novel Coronavirus (COVID 19; 2019-nCoV)
Coronaviruses (CoV) are a large family of viruses. This virus causes usually common cold to more severe diseases such as MERS-CoV (Middle east respiratory syndrome) and SARS-CoV (Severe acute respiratory syndrome). A novel coronavirus (n COV ) is a new human strain. As a result, we don’t have immunity against novel coronavirus.
In COVID 19, ‘CO’ stands for corona, ‘VI’ for virus, ‘D’ for disease. Coronaviruses are named as such because they look like little crowns under a microscope. In 2003 it was SARS. In 2012 it was MERS. Now in 2020 novel coronavirus was initially reported in December 2019 in the city of Wuhan in the Chinese province of Hubei. Coronaviruses are zoonotic. It is circulated in camels, cats and bats. The novel coronavirus transmitted from animal to human. Preliminary evidence suggests that the virus that causes COVID-19 may have originated in horseshoe bats in china.
SARS-COV was transmitted from civet cats to humans. Now transmission from snakes to rodents is possible.
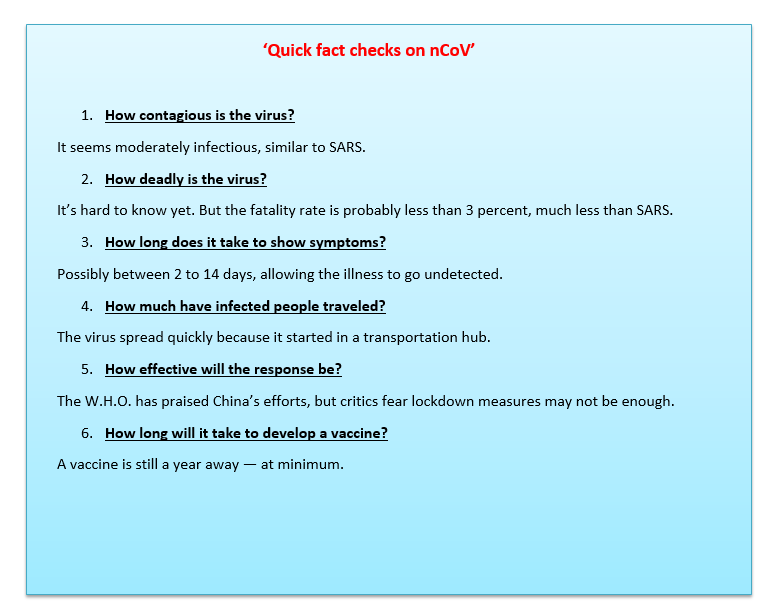
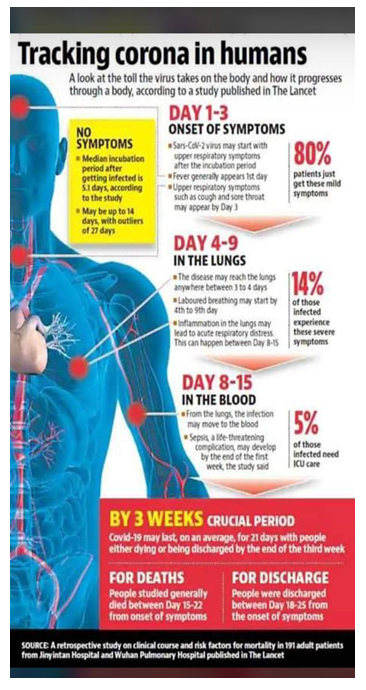
As per research published in the New England Journal of Medicine based on calculations the novel coronavirus has a Ro of 2.2 meaning each case patient could infect more than 2 other people. The study was based on first 425 cases of 2019 nCoV China. It also determined a mean incubation period of 5.2 days ( 2 – 14 days).
Common Human Coronaviruses
Common human coronaviruses including types 229E, NL63, OC43 and HKU-1 usually cause common cold like illness for a short amount of time.
Current outbreak of nCoV in China
As the coronavirus outbreak continues to spread across China, a flurry of early research is drawing a clearer picture of how the pathogen behaves and the key factors that will determine whether it can be contained. While the virus is a serious public health concern, the risk to most people outside China remains very low, and seasonal flu is a more immediate threat. To avoid any viral illness, experts advise washing your hands frequently and avoiding your office or school when you’re sick. Most healthy people don’t need masks and hoarding them may contribute to shortages for health workers who do need them, experts say.
If each person infected with the new coronavirus infects two to three others, that may be enough to sustain and accelerate an outbreak, if nothing is done to reduce it. The scale of an outbreak depends on how quickly and easily a virus is transmitted from person to person. While research has just begun, scientists have estimated that each person with the new coronavirus could infect somewhere between 1.5 and 3.5 people without effective containment measures.
That would make the virus roughly as contagious as SARS, another coronavirus that circulated in China in 2003 and was contained after it sickened 8,098 people and killed 774. Respiratory viruses like these can travel through the air, enveloped in tiny droplets that are produced when a sick person breathes, talks, coughs or sneezes. These droplets are larger than 5 microns in diameter and form a direct spray propelled upto 2 meters away from the infected person. Aerosol are droplets too but much smaller and may remain afloat for longer distances.
But the transmission numbers of any disease aren’t set in stone. They can be reduced by effective public health measures, such as isolating sick people and tracking individuals they’ve had contact with. When global health authorities methodically tracked and isolated people infected with SARS in 2003, they were able to bring the average number each sick person infected down to 0.4, enough to stop the outbreak. Health authorities around the world are expending enormous effort trying to repeat that.
How deadly is the virus?
It’s hard to know yet. But the fatality rate is probably less than 3 percent, much less than SARS.
This is one of the most important factors in how damaging the outbreak will be, and one of the least understood.
It’s tough to assess the lethality of a new virus. The worst cases are usually detected first, which can skew our understanding of how likely patients are to die. About a third of the first 41 patients reported in Wuhan had to be treated in an I.C.U., many with symptoms of fever, severe cough, shortness of breath and pneumonia. But people with mild cases may never visit a doctor. So there may be more cases than we know, and the death rate may be lower than we initially thought.
At the same time, deaths from the virus may be underreported. The Chinese cities at the center of the outbreak face a shortage of testing kits and hospital beds, and many sick people have not been able to see a doctor.
Early indications suggest the fatality rate for this virus is considerably less than another coronavirus, MERS, which kills about one in three people who become infected, and SARS, which kills about one in 10. All of the diseases appear to latch on to proteins on the surface of lung cells, but MERS and SARS seem to be more destructive to lung tissue. As of Jan. 31, fewer than one in 40 of the people with confirmed infections had died. Many of those who died were older men with underlying health problems.
SYMPTOMS
- Fever (83%) (Thermal scanners are effective in detecting people who have developed fever because of COVID- 19 infection)
- Cough (82%)
- Difficulty in breathing (31%)
- Mild gastrointestinal symptoms
- Sore throat
- Rhinorrhea
Complications
- Pneumonia is commonest (Bilateral pneumonia on imaging- 75%)
- Acute respiratory distress syndrome (29 %)
- Renal failure
- Acute cardiac injury (12%)
- Death
Complications are more common in people with cardio-pulmonary disease,Diabetes,weakened immune systems, infants and older adults ( age >6o year).
Death rates are lower in age less than 30 year.
DIAGNOSIS
1.Case Definition-
Suspect- Severe acute respiratory infection ( SARI) in a Person with history of fever and cough ,shortness of breath ( at least one sign/ symptoms of respiratory disease)requiring admission to hospital, with no other etiology that fully explains the clinical presentation AND any one of the following- 1, A history of travel to or residence in country/ area or territory reporting local transmission ( see NCDC website for an update list) of COVID 19 disease , 14 days prior to symptom onset OR The person develops an unusual or unexpected clinical course especially sudden deterioration despite appropriate treatment,without regard to place of residence or history of travel.
Probable
A person with acute respiratory illness of any degree of severity who within 14 days before onset of illness, had any of the following exposure-
- Close physical contact with a confirmed case of nCOV infection, while patient was symptomatic OR
- A healthcare facility in a country where hospital associated nCOV infections have been reported OR
- Direct contact with animals in countries where nCOV is known to be circulate in animal populations or where human infections have occurred as a result of presumed zoonotic transmission.
Laboratory diagnosis
The only diagnostic test to identify nCoV is RT-PCR.( Viral genome sequence)
Two consecutive negative PCR tests at least 24 hours remain gold standard.
C T Chest is a choice for pneumonia.
Difference between COVID-19 & Influenza
1.COVID-19 does not transmit as efficiently as influenza. The speed of propagation is different. The serial interval (the time between successive cases) for COVID-19 virus is estimated to be 5-6 days, while influenza virus serial interval is 3 days. This means that influenza can spread faster than COVID-19.
2.Patients transmit the virus at different times. Influenza virus transmission mainly occurs within 3-5 days after a person begins to develop symptoms and may spread before symptoms appear.
3.The contagious power is different.as per study COVID-19 pneumonia is more infectious than influenza and one patient can infect about 2 to 2.5 people. However, assessment of the infectivity of the two viruses is related to specific circumstance and time.
4.COVID-19 causes more severe disease (Mortality rate-3-4%) than seasonal influenza mortality (below 0.1%).
5.Children are important drivers of influenza virus transmission in the community. For COVID-19 virus, initial data indicate that children are less affected than adults and that clinical attack rates in 0-19 age groups are low. As per data from China children are usually affected by adults.
6.Those most risk for severe influenza infection are children, pregnant women, elderly with underlying chronic medical conditions and those who are immunocompromised. For COVID-19 as per current data older age and underlying conditions increase risk of infection.
7.For COVID-19 data suggest 80% of infections are mild or asymptomatic.15% severe infections requiring oxygen and 5% are critical infections , requiring ventilation.These fractions of severe and critical infection would be higher than what is observed for influenza infection.
8.Vaccines and therapeutic drugs available for seasonal flu but no specific drugs and vaccine currently licensed for COVID-19.
TREATMENT
- Symptomatic treatment.
- 2.Chloroquine, Tocilizumab, Interferon-alfa 2b, Remdesivir, Favipiravir, sarilumab drugs efficacy study done for COVID-19.
- As per Boston children Center protocol –
- Hydroxychloroquine (Need ID APPROVAL) - 13mg/kg/dose every 12 hourly x 2 for loading dose (max.400mg/dose or 800mg/day) followed by 6.5mg/kg/dose (max 400mg/day) for 4 days
- Azithromycin - 10mg/kg/day for 1 day then 5mg/kg for 4 days.
PREVENTION
1. Clean hands with soap and water for at least 20 seconds or alcohol-based hand rub.
2. Cover nose and mouth with tissue or inside elbow when coughing or sneezing.
3. Avoid close contact with anyone with cold or flu like symptoms
4. Throughly cook meat and eggs.
5. Avoid unprotected contact with live wild or farm animals.
6. Cover your cough or sneeze with tissue then throw tissue in trash.
7. N95 mask or Surgical mask for symptomatic cases.
6. schools are advised to avoid any large gathering of students during the course of the day inschool.
7. Social distancing - It is a public health practice that aims to prevent sick people from coming in close contact with healthy people in order to reduce opportunities for disease transmission. CDC define social distancing as it applies for COVID19 as “ remaining out of congregate setting , avoid mass gatherings maintaining distance ( approximately 6 feet or 2 meters) from other when possible.
8. Any student/staff with travel history to any COVID-19 affected country OR in contact with such person in the last 28 days should be monitored and home quarantined for 14 days.
Chemoprophylaxis with Hydroxychloroquine
The National Taskforce for COVID-19 recommends the use of hydroxy-chloroquine for prophylaxis of SARS-CoV-2 infection for selected individuals as follows:
Eligible individuals:
- Asymptomatic healthcare workers involved in the care of suspected or confirmed cases of COVID-19
- Asymptomatic household contacts of laboratory confirmed cases
Dose:
- Asymptomatic healthcare workers involved in the care of suspected or confirmed cases of COVID-19: 400 mg twice a day on Day 1, followed by 400 mg once weekly for next 7 weeks; to be taken with meals
- Asymptomatic household contacts of laboratory confirmed cases: 400 mg twice a day on Day 1, followed by 400 mg once weekly for next 3 weeks; to be taken with meals

