UPDATE
The New Seizure Terminology: How to Classify and Describe a Seizure
Active Epilepsy in Primary Care
Epilepsy is a disorder of the brain characterized by an enduring predisposition to having seizures, defined as episodes of abnormally excessive or synchronous neuronal activity in the brain, resulting in transient signs or symptoms.[1,2] Approximately 1.2% of the US population, or about 3.4 million people, have active epilepsy. Active epilepsy refers to a patient who is currently on antiepileptic medications and/or has had one or more seizures in the past year.[3,4]
Although there are healthcare providers who specialize in epilepsy-namely neurologists and epileptologists—only 53%–67% of patients in the United States with active epilepsy reported recently ("in the past year") seeing a neurologist or epileptologist.[5,6] Meanwhile, 86% reported recently seeing a general practitioner.[5]
Given that primary care providers are likely to see patients with seizures and epilepsy-some of whom may not be in the care of a neurologist or epileptologist-we would like to review the most current seizure terminology to help these clinicians better understand the different types of seizures and the importance of standardized terminology around seizures.
Accurate Seizure Classification
Accurately classifying different types of seizures using the latest standardized terminology is essential for several reasons. First, it allows healthcare providers and patients to accurately and effectively communicate with one another about seizure type using the same clear language. Second, some medications or therapies are more effective or only approved for specific seizure types and not others, so that errors in classifying seizure type may lead to ineffective treatment. Third, some types of drug-resistant seizures can effectively be treated by surgery, whereas others cannot. Fourth, current and future clinical research studies may have certain inclusion and exclusion criteria based on seizure type, so that knowledge of seizure type would be important prior to enrollment. Finally, accurate classification would lead to a better understanding of seizure type burden in the population, allowing various clinical, research, and public health resources to be allocated appropriately.
Historical Seizure Terminology
For centuries, seizures have been described using various terms. For instance, the terms "grand mal" (referring to seizures with bilateral tonic-clonic movements and loss of consciousness) and "petit mal" (seizures with behavioral arrest) have been used since the 1800s. With a better understanding of seizures and the advent of video electroencephalography (EEG), the International League Against Epilepsy (ILAE) published the first official classification of seizure types in 1981, introducing such terms as "partial vs generalized" and "simple vs complex." However, many of these historical terms have been criticized as being imprecise or nonspecific (eg, petit mal may refer to many different types of seizures with behavioral arrest) or confusing and misleading (eg, the term "partial" might suggest that a seizure was not a "full" one). With increasing knowledge, several iterations of ILAE's classification of seizure types have been published over the years to improve clarity, with the most recent being published in 2017.[17]
Current Seizure Terminology: Focal vs Generalized Onset
According to the current ILAE guidelines(available in many different languages), after first establishing that an event was likely a seizure by history and sometimes ancillary testing such as an EEG, the second task is to classify whether a seizure likely had a focal or generalized (or unknown) onset.[7,8](Figure 1)
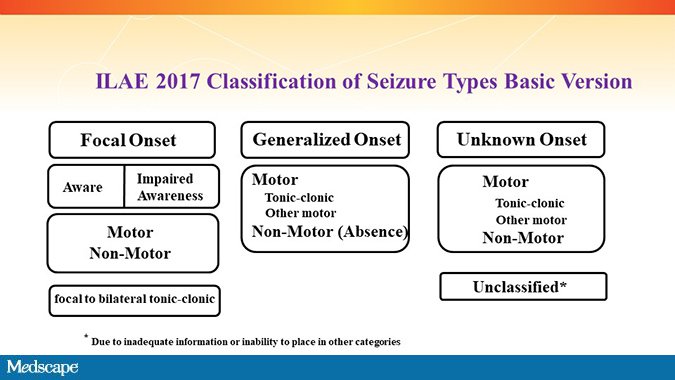
Figure 1. ILAE 2017 Classification of Seizure Types Basic Version.[7,8] From: Fisher RS, Cross H, French JA, et al. Instruction manual for the ILAE 2017 operational classification of seizure types. Epilepsia. 2017;58:531-542.
Focal-Onset Seizures
A focal-onset seizure-which may have previously been referred to as a "partial" seizure-is defined as a seizure originating in networks on only one side (hemisphere) of the brain. Generally, focality may be determined by the seizure presentation and any preceding symptoms, but other information from videos, EEG, or brain imaging may be useful as well. For instance, if a patient's typical seizure begins with right hand tingling and paresthesias, one could assume this was a focal-onset seizure originating from the left hemisphere. This might be further confirmed by an EEG showing epileptiform spikes or an electrographic seizure beginning in the left parietal lobe and/or an MRI showing a potential seizure-causing abnormality in that area. Sometimes the determination of focality is very clear based on history, clinical presentation, and ancillary tests, but at other times this may be more difficult and may require the help of a neurologist or epileptologist. Focal-onset seizures can be associated with acquired structural brain lesions and may begin in adulthood.
Generalized-Onset Seizures
A generalized-onset seizure is defined as a seizure originating at some point within and rapidly engaging bilaterally distributed networks on both sides (or hemispheres) of the brain. In other words, nearly the entire brain appears to be involved at the beginning of the seizure, based on clinical presentation or EEG. Now, this does not mean that there is not a focal site of onset of such seizures. Rather, it means that the seizure spreads so quickly that it is impossible to tell where it originated from using our current techniques. Because generalized-onset seizures involve both sides of the brain, there is almost always some level of impaired awareness or frank loss of consciousness in addition to other signs and symptoms. Generalized-onset seizures can be associated with metabolic derangements, channelopathies, or genetic syndromes and may begin in childhood.
Not uncommonly, a clear focal-onset seizure may eventually spread to the both sides of the brain, leading to loss of consciousness and bilateral tonic-clonic movements. In these cases, the initial symptoms or EEG suggest a clear laterality to the origin of the seizure, but the seizure then eventually spreads to both hemispheres. In the past this was called a "secondary generalized" seizure but is now referred to as a "focal-onset to bilateral tonic-clonic" seizure (to differentiate it from a generalized-onset seizure).
If there is limited information regarding a seizure, especially if it was unwitnessed, classifying it as either focal-onset or generalized-onset may be impossible. In this case, the seizure should be initially classified as having an unknown onset. Reclassification may be possible later with additional information.
Potentially useful questions to help with classifying a seizure include the following:
- Was this event likely a seizure or seizure mimic (eg, syncope, nonepileptic episode, etc.)?
- Did someone witness the event? If so, can they describe what happened?
- What were the initial symptoms or signs at the beginning of the event?
- Was there any loss of consciousness or awareness during the event?
- Was there any muscle shaking, stiffening, or loss of muscle tone during the event?
- Have these events happened before? If so, have the events happened the same way each time (ie, are stereotyped)? Or have different types of events occurred?
Of note, for simplicity, when classifying seizures, the word "onset" may not always follow the terms "focal" or "generalized." However, when "focal" or "generalized" are used, a reference to onset is always implied.
Current Seizure Terminology: Additional Optional Descriptors
Beyond classifying seizures into focal or generalized (onset), additional descriptors in the form of free text may be useful into better clarify the specific seizure type.
Awareness. With some focal-onset seizures, a patient may fully maintain awareness. Such seizures are now called "focal aware" seizures (abbreviated FAS, formerly "simple partial" seizures). With other focal-onset seizures, a patient's awareness may be impaired to a varying degree. Such seizures are now called "focal impaired awareness" seizures (abbreviated FIAS, formerly "complex partial" seizures). Impaired awareness is a surrogate marker for impaired consciousness. Although seizures are classified by their first manifestation, awareness is an exception, resulting in a FIAS if awareness is impaired at any time. Of note, describing level of awareness is typically only done for focal-onset seizures, as generalized-onset seizures almost always have impaired awareness or a frank loss of consciousness.
Motor components. Some seizures have a motor component and may simply be referred to as a "focal motor" seizure. However, more specific motor descriptions can be added, such as whether the motor seizure has automatisms (eg, lip smacking), an atonic component (loss of muscle tone), a myoclonic component (lightning-fast jerking movements), or a tonic and/or clonic component (formerly "grand mal" seizures), among other motor descriptors. Additionally, free text can be used to fully describe any unusual motor components.
Non-motor components. Other seizures have primarily a non-motor component and may simply be referred to as "focal non-motor" seizures. However, more specific non-motor descriptions can be added, such as whether the non-motor seizure is associated with sensory symptoms, cognitive symptoms, emotional symptoms, autonomic symptoms, behavioral arrest, etc. Additionally, free text can be used to fully describe any unusual non-motor components. Generalized non-motor seizures are essentially varieties of absence seizures, or what were called "petit mal" seizures in the past.
A complete list of the various optional seizure descriptors can be found in Figure 2.
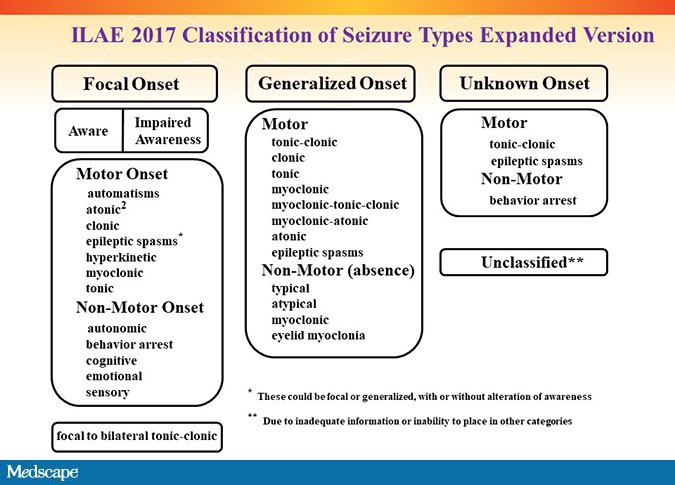
Figure 2. Optional seizure descriptors of behaviors in association with seizures. From: Fisher RS, Cross H, French JA, et al. Instruction manual for the ILAE 2017 operational classification of seizure types. Epilepsia. 2017;58:531-542.
Challenges and Future Directions
The current 2017 ILAE classification of seizure types is based on the best knowledge of seizures at this time. However, advances in EEG, imaging, and/or other testing may justify further refinements to these classifications in the future. Classification of the epilepsies and epilepsy syndromes is beyond the scope of this article.
Unfortunately, ICD-10 coding terminology has lagged behind the most recent ILAE seizure classifications. For instance, ICD-10 uses the terms "simple partial" and "complex partial" with some seizure codes. We hope (and encourage) that future versions of the ICD coding system will better align with the latest ILAE seizure terminology.
- Seizures should be classified mainly on whether they have a focal onset or a generalized onset, because etiology, treatment, and prognosis may differ between these two types.
- Additional descriptors regarding awareness, motor, and non-motor symptoms may be added (but are optional).
- The terms "simple partial," "complex partial," "petit mal," and "grand mal" are outdated and should no longer be used routinely to describe seizure types.
- The current ILAE terminology and ICD-10 code version are still not fully concordant but hopefully will improve with subsequent ICD code versions.
References
- Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46:470-472. Abstract
- Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475-482. Abstract
- Centers for Disease Control and Prevention. Epilepsy. Source Accessed August 1, 2018.
- Zack MM, Kobau R. National and state estimates of the numbers of adults and children with active epilepsy—United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:821-825. Abstract
- Centers for Disease Control and Prevention. Epilepsy in adults and access to care-United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:909-913. Abstract
- Tian N, Boring M, Kobau R, Zack M, Croft J. Active epilepsy and seizure control in adults - United States, 2013 and 2015. MMWR Morb Mortal Wkly Rep. 2018;67:437-442. Abstract
- Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58:522-530. Abstract
- Fisher RS, Cross JH, D'Souza C, et al. Instruction manual for the ILAE 2017 operational classification of seizure types. Epilepsia. 2017;58:531-542. Abstract
Source: https://www.medscape.com/viewarticle/904131?nlid=126320_455&src=WNL_mdplsfeat_181127_mscpedit_peds&uac=89597BG&spon=9&impID=1813859&faf=1

