Web Watch
Is antibiotic exposure during pregnancy and/or during early childhood associated with the development of childhood obesity?
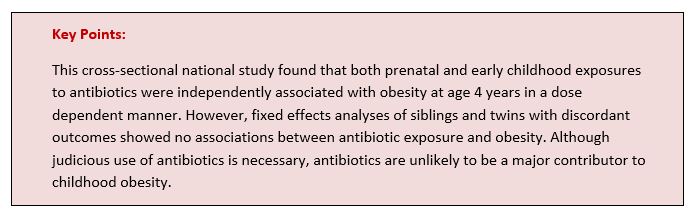
OBJECTIVE: Although antibiotics are associated with obesity in animal models, the evidence in humans is conflicting. To assess whether antibiotic exposure during pregnancy and/or early childhood is associated with the development of childhood obesity, focusing particularly on siblings and twins.
DESIGN, SETTING, AND PARTICIPANTS: This cross-sectional national study included 284 211 participants (132 852 mothers and 151 359 children) in New Zealand. Data analyses were performed for 150 699 children for whom data were available, 30 696 siblings, and 4188 twins using covariate adjusted analyses, and for 6249 siblings and 522 twins with discordant outcomes using fixed effects analyses. Data analysis was performed November 2017 to March 2019.
EXPOSURE: Exposure to antibiotics during pregnancy and/or early childhood.
MAIN OUTCOMES AND MEASURES: The main outcome is odds of obesity at age 4 years. Anthropometric data from children born between July 2008 and June 2011 were obtained from the B4 School Check, a national health screening program that records the height and weight of 4-year-old children in New Zealand. These data were linked to antibiotics (pharmaceutical records) dispensed to women before conception and during all 3 trimesters of pregnancy and to their children from birth until age 2 years.
RESULTS: The overall study population consisted of 132 852 mothers and 151 359 children (77 610 [51.3%] boys) who were aged 4 to 5 years when their anthropometrical measurements were assessed. Antibiotic exposure was common, with at least 1 course dispensed to 35.7%of mothers during pregnancy and 82.3%of children during the first 2 years of life. Results from covariate adjusted analyses showed that both prenatal and early childhood exposures to antibiotics were independently associated with obesity at age 4 years, in a dose-dependent manner. Every additional course of antibiotics dispensed to the mothers yielded an adjusted odds ratio (aOR) of obesity in their children (siblings) of 1.02 (95%CI, 0.99-1.06), which was similar to the odds across pregnancy for the whole population (aOR, 1.06; 95%CI, 1.04-1.07). For the child’s exposure, the aOR for the association between antibiotic exposure and obesity was 1.04 (95%CI, 1.03-1.05) among siblings and 1.05 (95%CI, 1.02-1.09) among twins. However, fixed-effects analyses of siblings and twins showed no associations between antibiotic exposure and obesity, with aORs of 0.95 (95%CI, 0.90-1.00) for maternal exposure, 1.02 (95%CI, 0.99-1.04) for child’s exposure, and 0.91 (95%CI, 0.81-1.02) for twins’ exposure.
CONCLUSIONS AND RELEVANCE: Although covariate-adjusted analyses demonstrated an association between antibiotic exposure and odds of obesity, further analyses of siblings and twins with discordant outcomes showed no associations. Thus, these discordant results likely reflect unmeasured confounding factors. (JAMA Network Open. 2020;3(1):e1919681. doi:10.1001/jamanetworkopen.2019.19681)