How to make U.P. India’s pride?
The disease and the prescription!
The real India?
We live in a nation that is characterized by extreme diversity. Diversity in every sense, in every sphere. Be it religion, cast, creed, culture, tradition, language, environment, social milieu, eating habits, and economic strata. Sometimes, one wonders what represents the real India! Then, there is this impression of co-existence of ‘two nations’ within one -‘India’ versus ‘Bharat’ divide! The former is exemplified by all its development, highly educated, upwardly mobile, highly ambitious, competitive, elite and wealthy population and the latter stricken with poverty, illiteracy, unemployment, hunger, ignorance, struggling hard to come to terms with mere survival. The one is a progressive, vibrant, rapidly evolving economy destined to become next super power; the other is a flail and a failed nation that is regressive, orthodox, and underdeveloped! So the question remains-where lies real India? If we for the time being put aside this two nation divide, one need not to stretch their imagination further to look out for the answer. Yes, it is the ‘Hindi-heartland’ that symbolizes the real India in every sense! And even in this broad chunk, Uttar Pradesh comes closest to represent its country. It would not be a hyperbole to proclaim U.P. as the heartland of India. But, despite representing the real state, despite being the most populous state of the country, and despite being the most sensitive political state of the country, the irony is U.P. is a sick state today! How on earth a country can progress, prosper or even pulsate when its heart is diseased?
The plight of UP’s kids:
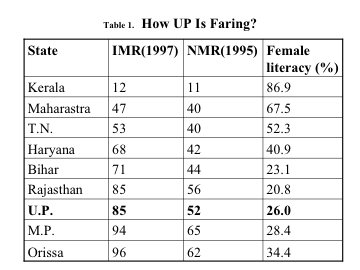
U.P. is lagging behind on many fronts. Whether it is economic growth, educational status of its polity, productivity, industrialization, infrastructure, population density, status of women and children and other demographic indices. And health is no exception. ‘Infant Mortality Rate’ (IMR) is the most sensitive indicator of the overall health of a society, state or a country. U.P. is lying almost at the bottom of the table along with other ‘Bimaru’ states as far as IMR is concerned. The plight of UP’s children is overtly visible-be it any static health index or disease specific data or the immunization status of the target pediatric population. Though the state is grappling with controlling the known vaccine-preventable diseases like polio, measles, pertussis, certain diseases extinct elsewhere in the country like diphtheria and neonatal tetanus are regularly reminding the caretakers of UP’s health that there is grossly inadequacy of a competent health delivery system in the state. The situation is further compounded by almost regular occurrences of epidemics of some known brain diseases (like JE in eastern UP) and some not so known diseases (epidemic encephalopathy in western UP). And, we have not discussed the plight of neonatal health as yet- dying in thousands daily! Anemia, malnutrition, stunting and other chronic diseases are no less a burden. Burning issues of more developed states like child labor, child abuse and neglect, and many other psychosocial ills of adolescents are still not a priority in the state. UP is still not prepared to lend its ears to all these aberrations of a mature, urbanized and advanced society.
The crux of the problem:
If one seriously analyzes the reasons of state’s deteriorating health, the peculiar demographic milieu of the state should take the brunt of the blame. Demographically UP is vulnerable to onslaught of many-many diseases (Table 1). Do you know UP is adding another Canada, another Australia and New Zealand to its population every 10 years? How can any state prosper without being properly compensated economically to match its population overgrowth! All the ills state facing today can be summarized through ‘UIP’-where ‘U’ signifies unchecked population growth, unemployment, and unhygienic living conditions, ‘I’ illiteracy and ignorance, and ‘P’ poverty, political mismanagement and poor public health. All these drawbacks coupled with corruption, community indifference toward health, coordination failure amongst various agencies manning health, callous attitude of health administration, and complacency amongst them have further contributed to deteriorating child health in the state.
Table 2. Population distribution, percentage decadal growth, sex ratio, population density and literacy rate:
|
National/State/UT |
Population |
Percentage Decadal Growth (91-01) |
Sex Ratio (females per 1000 males |
Population density (Per Sq. Km.) |
Literacy rate |
|
India |
1,027,015,247 |
21.34 |
933 |
324 |
65.38 |
|
U.P. |
166,052,859 |
25.80 |
898 |
689 |
57.36 |
|
Kerala |
31,838,619 |
9.42 |
1,058 |
819 |
90.92 |
|
Maharashtra |
96,752,247 |
22.57 |
922 |
314 |
77.27 |
|
West Bengal |
80,221,171 |
17.84 |
934 |
904 |
69.22 |
The glimmer of hope:
The only ‘plus point’ quite paradoxically UP can boast off is its extremely vicarious situation as a most poorly performing state of the country. The fact that UP lies in the bottom of all health related indicators and having highest number of sick children in the country gives it some hope of salvaging its situation. As you know, only two broad groups grab the attention-the one sitting at the top and the other lying in the bottom! UP might give the nation, health experts, administrators, international health agencies, NGOs, community, corporate world, and all those entrusted with the job of health management a chance to showcase their abilities to catapult a sick state in to one of the healthiest states of the country!
What are the solutions, then?
There are no easy solutions to improve health of the state. Nor there is any magic bullet to change the doomed scenario overnight. It calls for concerted all out efforts at many fronts.
1-Making health a political issue.
It took the ongoing epidemic of JE in eastern UP that has already killed more than 1,000 children this year alone and might have killed more than 10,000 in last 25 years to shake not only the health agencies, state government and political parties but the central government also from their inertia. For the first time, any health issue seems to become a political issue. But for how long?
So far health and health related issues are not considered as viable, potent political tools. And quite ostensibly the issues, which ideally would not have been any issues, like caste, creed, religion, nepotism, etc are taking central place. In every election manifesto, issues related to health are either not enlisted or not given any priority if they are mentioned. Until the health issues are made ‘political planks’ in every state election be it panchayat, municipal, assembly, or parliamentary all our efforts to make UP a model healthy state would go in vain.
2-Professional management of existing public health delivery system.
As far as the infrastructure of public health delivery system is concerned, quite surprisingly it has got and excellent framework (Fig.1). But, sadly, most of the public premises are in poor state. In a state of ruins and lying in shambles! If anyone wishes to even entertain the idea of improving UP’s health, the first and foremost task would be to vastly revamp the existing functioning of these public health outlets with a liberal dose of professional, corporate-like management. Even privatization of public health in the state would not be an altogether absurd idea. After all, we need a health delivery system which is not only sensitive, affordable and accessible but also competent and efficient also .
.png)
3-Greater engagement of health agencies and NGOs.
So far, the contribution made by various national and international health agencies, NGOs, and academic bodies has been quite negligible. This is indeed a disappointing situation considering the magnitude of the problems dogging child health in the state and the scope for participation by this sector. Still, 99.9% health schemes and child welfare programs are being run solely by the government owned public sector. The need of the hour is all out massive involvement of this sector in the child health development activities. The NGOs would need to display far greater urgency, seriousness, sincerity, and sensitivity and greater resolve to face the challenge. They ought to shed their tendency to project ‘rosy postcard’ image of Indian children rather than should concentrate on ground realities and streamline their energy to alleviate sufferings of millions of hapless children.
4-Health insurance schemes.
This practice widely prevalent in developed world would need to be implemented on a mass basis all over the state especially targeting the poor, rural population. Though GOI has initiated this scheme in few selected regions, but to make an impact the government would need to invest heavily in this sector.
5-Highest priority to neonatal-maternal health.
Neonatal health is probably the most neglected area of public health in the state. Even society does not accord any significance to the survival and well being of a neonate. Surprisingly, pregnancy and birth of a newborn are regarded as essential rituals but not the survival of a neonate! It is abundantly clear that if UP or for that matter any other poorly performing state of the country has to make any serious attempt to reduce their bloated mortality figures, they would need to give neonatal and maternal health the highest priority. Of late, government has also recognized the significance of neonatal survival and accorded a high priority to neonatal and maternal health in its next RCH program through launching IMNCI scheme. If one seriously estimates the neonatal mortality per day in the state, the figure would run in thousands! So one can imagine the enormous human loss as well as the massive wasteful expenditure of the society on the rituals of pregnancy and childbirth. Most government run health centers lack proper equipment and requisite expertise to deal with neonatal problems. Hence, to achieve the target of low NMR/IMR in the state, not only the revamping of these centers is required but the society should also need to change their mindsets toward neonatal survival.
6- Mass awakening about child health and survival:
As elaborated above, sensitization of the public through effective IEC regarding various child health issues is one intervention that can be utilized at community level. For example, IEC regarding essential newborn care, vaccination, breastfeeding, safe motherhood, prevention of anemia, nutritive values of different foods and their role in prevention of malnutrition and anemia etc are few of the theme issues that can be taken up. Here again, NGOs can help the public health administrators.
7- Involvement of corporate world in public health:
Corporate sector should be urged to invest in public health. They need to be convinced about the viability of low cost, professionally managed, subsidized ‘Janta Hospitals’ in the rural/remote areas of the state to provide essential medical care at primary level.
8- Innovative measures:
Time has come to take certain bold, path breaking steps to boost child health in the state in a big way. Few such steps are enlisted below:
# Vaccination drive against major VPDs can be amplified by creating “Vaccination pickets” in every nook and corner of the state with round the year availability of all UIP vaccines. Complete vaccination before admission in any primary school should be made compulsory.
# ‘Certificate courses’ on key child health promotional issues for the class X/XII students should be initiated especially in vulnerable areas. Greater emphasis should be given to these issues in academic curriculum.
# Every attempt should be made to exploit all existing health delivery contacts such as RMPs, GPs and even quacks in the remote areas. Limited training and orientation courses in key community health issues like management of common childhood diseases, role of breastfeeding and ORS, essential newborn care etc should be provided to them.
# Every district hospital should be instructed to maintain a mortality/morbidity database of their respective districts, which should be periodically evaluated by independent agencies.
# As polio eradication program is fast approaching to its conclusion, services of the representatives of NPSP network and Unicef can be obtained in the monitoring of different childhood ailments.
# Positive involvement of the media acts as a catalyst to administration, politicians and health department. They should be taken in to confidence on initiation of any new child health initiative and urged to disseminate IEC on child health issues.
# Better perks, early promotion and more financial incentives should be provided to health professionals agreeing to work in rural sector.
# Adequate investigational facilities along with interlinking with state level laboratories, and sufficient equipments in working condition should be made available at every public health outlet.
# At village, block and city level, ‘gram pradhans’, panchayat members, block pramukh, municipal board members, city municipal chairman or mayor, should be made accountable for vaccination and other child health promotional activities of their respective zones.
# At district and commissionary level, commissioners, district magistrates, CMOs and other top district administrators should be assigned the job of supervising child health related programs in their areas. Certain targets like attaining a 25% reduction in IMR in a stipulated time frame should be fixed. Regular reviews of the child health status as done with polio eradication program need to be instituted.
# At the state level, the Chief secretary and Chief minister should directly supervise implementation and progress of different child health welfare programs in the state. A ‘UP Chikitsa Parishad’ under the aegis of Chief minister office can be formed to monitor and provide impetus to all child health schemes in the state. The members of the parishad can be state representatives of health agencies, NGOs, academic bodies, prominent business houses, prominent sports celebrity, and media persons apart from state health experts and bureaucrats.
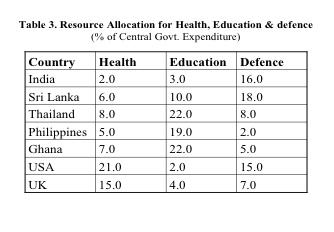
# At the national level, advocacy to provide more budgetary allocation to state for investment in child health should be initiated. Table 3 depicts the current expenditure by central government on health in comparison to defense and education,
# At the international level, intense lobbying should be done to project UP as one of the most vulnerable and precariously placed state of the world in regard to child health. Various international donor agencies should be convinced about the urgent need of investing in public health in the state.
9-Medical colleges should play more proactive role:
Barring few most of the state medical colleges are facing a crisis as far as faculty, infrastructure and equipments are concerned. Hardly any quality community oriented research work is being done at most of these centers. There is an urgent need to greatly revamp at least the pediatrics and community medicine departments of all state medical colleges so that they could regain their regional nodal center status of yore. HODs of pediatrics should instruct their PG students to undertake some research work that has direct bearing on the health status of local pediatric community. Community oriented projects should be given priority to generate indigenous data on which future region specific recommendations should base upon.
10- Improvement of poor demographic profile:
All the above-mentioned interventions and measures might fail or would not be needed at all if the root cause of this messy affair is dealt with some seriousness. The three basic issues of poverty, illiteracy and population overgrowth would need to be dealt with at some time or other. Though this approach may take another 2-3 decades to achieve the objectives but the results would be more long lasting. After all, health is not a static state. To make the state healthy for forever, it needs not merely more healthcare nor more health professionals but above all a healthy environment with enough space to breath and survive coupled with economic well being to sustain the benefits of good health- both physical and mental. The state should not hesitate in taking even some harsh, coercive measures to ensure that the basic demographic anomalies are corrected at the earliest.
11-Role of IAP and other professional bodies:
The first and foremost objective of these academic bodies should be the advocacy. Advocacy on every aspect of child health should be the main aim. They should also regularly issue recommendations on disease specific interventions at community level not only to their members but to health planners of the state also. Office bearers and members of these organizations should exhort government and their representatives to give highest priority to health and health issues of the community. They need to work in tandem with other agencies engaged in the field of child survival. IAP through its vast network of local branches should help local health administration in IEC on common health problems of children of their areas. Individual member can also chip in by devoting some time on regular interval to charitable community oriented work, such as providing free vaccination, organizing health check camps, adopting a backward slum/rural area and ensuring complete vaccination and subsidized treatment to common ailments etc. A sort of public-private partnership is the need of the hour.
Conclusion:
Making UP a healthy and disease free state is not an easy task. It calls for an all out efforts to match the performance of more advanced, well performing states of the country. Bringing health to the forefront of political agenda, increasing budgetary allocation to health, generous support from national and international donor agencies, professional management of existing health infrastructure, introduction of health insurance, concerted coordinated efforts through better public-private partnership, involvement of corporate sector in health care at peripheral level, assigning responsibility and accountability to public representatives, constructive involvement of media and academic bodies, revamping of public health outlets are the few key interventions that can help the state realize its dream of making Uttar Pradesh an ‘Uttam Pradesh’. At least, in regard to child health.
The setting up of the ‘National Rural Health Mission’ (NRHM) by the central government with an allocation of about Rs 6,700 crores to step up public expenditure in healthcare from 0.9% to 2-3% is welcome gesture. Its recommendation to increase retirement age of doctors to 65 years and introducing a compulsory stint for them in rural areas are steps in right direction. But, it would be naïve to believe that an army of doctors is a magic remedy for all the ills affecting public health of the state today. We need to attack the root causes-poverty, illiteracy and overpopulation to make health as permanent possession of the state.
Bibliography:
1-Uttar Pradesh demography. Government of Uttar Pradesh. Official website of Government of UP. Available at: http://www.upgov.nic.in/upinfo/sandc.html
2-Central Government Health Schemes. Official website of Ministry of Health and Family Welfare. Available at: http://www.mohfw.nic.in/reports/index.htm
3-State of India’s Newborns. National Neonatology Forum & Save the Children/US. November 2004, New Delhi-Washington, DC.
4- Bhakoo ON, Kumar P. Milestones in Neonataology in India. In Guha’s Neonataology Principles and Practice, 3rd edn, 2005. Editors Arvind Saili, Swarnarekha Bhat, Arvind Shenoi, Jaypee, New Delhi,
5- Singh M. The current status and challenges of perinatal services in India. In Care of Newborn, 6th edn 2004, Ed Meharban singh, Sagar publication, New Delhi.

